Back to Journals » Clinical Ophthalmology » Volume 8
Histopathological examination of Acanthamoeba sclerokeratitis
Authors Kato K , Hirano K , Nagasaka T, Matsunaga K, Takashima Y, Kondo M
Received 22 September 2013
Accepted for publication 23 October 2013
Published 16 January 2014 Volume 2014:8 Pages 251—253
DOI https://doi.org/10.2147/OPTH.S54807
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Kumiko Kato,1 Koji Hirano,2 Tetsuro Nagasaka,3 Koichi Matsunaga,1 Yuko Takashima,1 Mineo Kondo1
1Department of Ophthalmology, Mie University School of Medicine, Tsu, Japan; 2Department of Ophthalmology, Fujita Health University, Nagoya, Japan; 3Department of Medical Laboratory Science, Nagoya University Graduate School of Medicine, Nagoya, Japan
Purpose: To report the histopathological findings in a case of severe Acanthamoeba sclerokeratitis (ASK).
Patient and methods: A 46-year-old patient was referred to the Department of Ophthalmology of Mie University Hospital because of a severe corneal ulcer of the right eye of 6 months' duration. Our initial examination showed a ring-shaped corneal opacity with extensive epithelial defects and nodular scleritis. Cysts of Acanthamoeba were identified in cultures from corneal scrapings, and he was diagnosed with ASK. He was started on antiamoebic treatment, including topical micafungin and chlorhexidine. The corneal ulcer was debrided several times. One month later, he developed necrotizing scleritis, and the cornea suddenly perforated. The eye was enucleated because of severe pain and prepared for histopathological examination.
Results: The histopathological examination showed an infiltration of polymorphonuclear leukocytes throughout the corneal stroma and also in the limbal area of the sclera, forming an abscess. Granulation tissue was observed in the anterior sclera close to the ciliary body, but the posterior regions of the eye were not affected by inflammation or tissue destruction. The cysts of Acanthamoeba were observed only in the cornea.
Conclusion: Histopathological examination of an eye with severe ASK showed that the inflammation and tissue granulation were present only in the anterior part of eye, and the posterior segment was not affected. Because the inflammation and tissue destruction were confined to the anterior segment, enucleation might not have been necessary if the severe pain was able to be controlled.
Keywords: Acanthamoeba sclerokeratitis, histopathology, acute and chronic inflammation, enucleation
Introduction
Acanthamoeba sclerokeratitis (ASK) is a rare and severe complication of advanced Acanthamoeba keratitis (AK), and it has been estimated to occur in 14%–16% of AK cases.1,2 Despite intensive antiamoebic therapy, the prognosis of ASK is poor, and it occasionally requires enucleation, mainly because of the intense pain in a blind eye.3,4
The pathogenesis of ASK is poorly understood. It is still not known whether this severe scleral inflammation is induced by an immune-mediated reaction secondary to AK or a direct invasion of Acanthamoeba into the sclera.
We examined a patient with ASK whose eye had to be enucleated because of corneal perforation and severe pain. Histopathological examinations of the enucleated eye showed that the pathological findings were confined to the anterior segment, and the posterior segment was completely normal.
Case report
A healthy 46-year-old man was referred to our hospital with severely reduced vision and severe pain to have his eye examined. He had been diagnosed with herpetic disciform keratitis at a local clinic 6 months earlier because of a ring infiltrate. Because of complications of iridocyclitis, he was treated with topical and systemic steroids along with acyclovir ointment. However, the symptoms and findings worsened, and he was referred to our hospital.
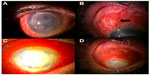
On his first visit, we learned that he had been wearing 1-day disposable soft contact lenses for several days. The visual acuity in his right eye was hand motion, and the cornea had a ring-shaped opacity with extensive epithelial defects (Figure 1A). A nodule was observed beneath the highly injected conjunctiva at the superior sclera close to the limbus (Figure 1B, arrow). Cysts of Acanthamoeba were identified in cultures of samples of the corneal abscess, and the patient was diagnosed with ASK. He was treated with oral itraconazole and topical micafungin and chlorhexidine (0.02%) hourly. The corneal region was debrided several times; however, the injection of the conjunctiva and sclera worsened, leading to necrotizing scleritis 1 month after the first examination (Figure 1C). An 8 mm-diameter ring-shaped abscess developed in the corneal lesion, and soon after that the cornea perforated (Figure 1D). Because he complained of severe pain and requested removal of the right eye, the eye was enucleated under general anesthesia.
Paraffin sections of the enucleated eye were examined histopathologically. Cysts of Acanthamoeba and polymorphonuclear leukocytes (PMNLs) were observed throughout the corneal stroma, indicating an active invasion of the protozoan (Figure 2B). The anterior sclera in the limbal area was acutely inflamed with an infiltration of PMNLs, and an abscess was observed at the limbus (Figure 2B and C). However, the sclera close to the ciliary body appeared different: granulation tissue consisting of congested blood vessels surrounded by macrophages and lymphocytes was observed in this area (Figure 2D). Interestingly, the signs of inflammation and granulation were not observed in the sclera posterior to the insertion of the rectus muscles or in the retina or choroid.
Discussion
Several cases of ASK have been reported, and 5 out of the 11 cases, found the eyes were enucleated.1,3–8 Histopathological evaluations of these eyes showed that cysts of Acanthamoeba were observed in the scleral region in only 2 eyes.3,5 Dougherty et al3 reported that the cysts were associated with inflammatory cells, eg, lymphocytes, plasma cells, and histiocytes, deep in the anterior sclera. These findings suggested that it may be difficult to treat ASK by topical antiamoebic drugs. Ebrahimi et al5 also detected cysts in the limbal area, and suggested a direct invasion of Acanthamoeba from the cornea.
The eye from our case study had histopathological features of acute and chronic inflammation in the anterior segment. The cornea was infiltrated by PMNLs and cysts of Acanthamoeba over a large area, suggesting highly active AK even 6 months after the onset of AK and active treatment with antiamoebic drugs. The abscess was present in the limbal area, and granulation tissue with diffuse invasion of monocytes was seen in the deep sclera close to the ciliary body. Despite these severe inflammatory findings in the anterior part of the eye, we could not find any evidence of inflammation or tissue destruction in the sclera posterior to the insertion of the rectus muscle or in the retina or choroid. We assumed that the absence of vessels in the cornea and the difference in the blood supply to the anterior and posterior parts of the sclera accounted for the histopathological differences. Although we could not find any cysts or trophozoites of Acanthamoeba in the scleral area, the abscess and the granulation tissue observed in the anterior sclera strongly indicated that there should be microorganisms and granulation tissue in the scleral regions.
Enucleation is occasionally performed because of suspected endophthalmitis in eyes with severe microbial keratitis.9 However, as our case demonstrated, inflammation and tissue destruction might be confined to the anterior segment, and the posterior part of the eye can remain normal even in eyes with severe ASK. We suggest that enucleation or evisceration can be avoided in these ASK cases if the severe pain can be controlled. Systemic steroids or immunosuppressives are suggested to suppress inflammation and to relieve pain for ASK patients.4,6,8 However, we have to be aware that cysts of Acanthamoeba are still in the corneal region, and both topical and systemic antiamoebic therapy should be continued together with systemic immunosuppressive therapy.
In our case, a delay in the diagnosis of AK and the application of topical steroids might have led to the ASK. Thus, we should be aware that AK can resemble herpetic keratitis,1,10 and topical steroids should be used more discreetly for keratitis of unknown origin.
Disclosure
The authors report no conflicts of interest in this work.
References
Mannis MJ, Tamaru R, Roth AM, Burns M, Thirkill C. Acanthamoeba sclerokeratitis. Determining diagnostic criteria. Arch Ophthalmol. 1986;104(9):1313–1317. | |
Bacon AS, Frazer DG, Dart JK, Matheson M, Ficker LA, Wright P. A review of 72 consecutive cases of Acanthamoeba keratitis,1984–1992. Eye (Lond). 1993;7(Pt 6):719–725. | |
Dougherty PJ, Binder PS, Mondino BJ, Glasgow BJ. Acanthamoeba sclerokeratitis. Am J Ophthalmol. 1994;117(4):475–479. | |
Kuennen RA, Smith RH, Mauger TF, Craig E. Enucleation following treatment with intravenous pentamidine for Acanthamoeba sclerokeratitis. Clin Ophthalmol. 2010;4:1145–1149. | |
Ebrahimi KB, Green WR, Grebe R, Jun AS. Acanthamoeba sclerokeratitis. Graefes Arch Clin Exp Ophthalmol. 2009;247(2):283–286. | |
Lee GA, Gray TB, Dart JK, et al. Acanthamoeba sclerokeratitis: treatment with systemic immunosuppression. Ophthalmology. 2002;109(6):1178–1182. | |
Hirano K, Sai S. Severe Acanthamoeba sclerokeratitis in a non-contact lens wearer. Acta Ophthalmol Scand. 1999;77(3):347–348. | |
Pineda R 2nd, Kocatürk T, Bhui RD. Visual outcome and rehabilitation in a case of bilateral Acanthamoeba sclerokeratitis. Cornea. 2007;26(9):1150–1152. | |
Cruz CS, Cohen EJ, Rapuano CJ, Laibson PR. Microbial keratitis resulting in loss of the eye. Ophthalmic Surg Lasers. 1998;29(10):803–807. | |
Lindquist TD. Treatment of Acanthamoeba keratitis. Cornea. 1998; 17(1):11–16. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.