Back to Journals » Open Access Journal of Sports Medicine » Volume 6
Family medicine residents’ perceived level of comfort in treating common sports injuries across residency programs in the United States
Authors Amoako A, Amoako A, Pujalte G
Received 20 July 2014
Accepted for publication 12 September 2014
Published 23 March 2015 Volume 2015:6 Pages 81—86
DOI https://doi.org/10.2147/OAJSM.S71457
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Freddie H Fu
Video abstract presented by Adae Opoku Amoako
Views: 100
Adae O Amoako,1 Agyenim B Amoako,2 George GA Pujalte3
1Department of Family and Community Medicine, Penn State Hershey Medical Center, Hershey, PA, USA; 2Department of Family Medicine, University of Arkansas for Medical Sciences Northwest, Fayetteville, AR, USA; 3Sports Medicine, Divisions of Primary Care, and Orthopedics, Mayo Clinic Health System, Waycross, GA, USA
Background and objective: Family physicians are expected to be comfortable in treating common sports injuries. Evidence shows a limited level of comfort in treating these injuries in pediatric and internal medicine residents. Studies are lacking, however, in family medicine residents. The purpose of this study is to assess the comfort level of family medicine residents in treating common sports injuries in adults and children based on their perceived level of knowledge and attitudes.
Methods: This is a cross-sectional study of family medicine residents in the United Sates. A written survey of 25 questions related to sports injury knowledge and factors affecting comfort level were collected. A chi-square test was implemented in calculating P-values.
Results: Five hundred and fifty-seven residents responded to the survey. A higher percentage of doctors of osteopathy (86.6%, 82.5%, 69.6%, and 68.7%) compared to doctors of medicine (78.5%, 71.6%, 53.4%, and 52.8%) respectively identified ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis as common injuries, and felt comfortable in treating them (P-values =0.015, 0.004, 0.0001, and 0.0002, respectively). Residents with high interest in sports medicine correctly identified the injuries as common and felt comfortable treating them as well (knowledge, P=0.027, 0.0029, <0.0001, and 0.0001, respectively; comfort level, P=0.0016, <0.0001, 0.0897, and 0.0010, respectively).
Conclusion: Medical education background, factors that affect training, and an interest in sports medicine contribute to residents' knowledge and comfort level in treatment of common sports injuries.
Keywords: athletic injuries, graduate medical education, sports medicine
Introduction
More than 35 million children participate in organized sports, and even more participate in unorganized sports.1 The yearly cost for treating injuries sustained while participating in such activities in children is estimated to be as high as $1.8 billion.2 There are an estimated 4.3 million emergency visits for sports-related injuries each year in both adults and children.3 Sports injuries in children account for the majority of the over ten million injury-related primary care office visits annually in the United States.4 These figures underline the importance of sports medicine as a primary care subspecialty; therefore, it would seem logical to expect family physicians to be comfortable treating common sports-related injuries when they are encountered in the office.
Studies have shown that training in musculoskeletal medicine is inadequate in both medical school and non-orthopedic residency training programs.5 The question, therefore, is whether or not family medicine residents are ready to tackle the common sports injuries that they would be exposed to after residency training. In 2004, it was shown that the traditional curriculum of family medicine would not be able to meet the needs of the future,6 and there have been discussions on whether the length of time in training may be the culprit.7 The suggestion to increase the length of family medicine residency training to 4 years has been one focal point in this discussion. Some programs are experimenting with this idea, although the verdict remains divided.8,9
In pediatric and internal medicine residencies, studies have identified suboptimal sports medicine training and low comfort level in treating common injuries.10,11 However, the current available literature does not appear to include any studies investigating the comfort level of family medicine residents in treating common sports injuries. We hope this study will be a good starting point for future studies.
Methods
This is a cross-sectional study of residents across the United States in all ACGME- and American Osteopathic Association (AOA)-accredited family medicine programs between July and October 2013. Programs were selected from the American Medical Association’s Fellowship and Residency Electronic Interactive Database Access (FREIDA) list of all ACGME-accredited programs and the AOA’s database of approved osteopathic residency programs. The email addresses of 413 program coordinators and directors were obtained, and an email with a link to an online survey of 25 questions related to residents’ perceived sports injury knowledge, factors affecting their comfort level, and their views on current sports medicine training were sent to be disseminated to residents. Questions included medical degree type, region of United States where residency was located, and history of participation in competitive sports. The survey questions were grouped into three categories. The first category contained knowledge-based and comfort-level questions on ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis. The second category contained questions about factors that pertained to the residents’ training which included average number of sports-related injuries exposed to, patient population (lower class, middle class, or affluent), location of residency (rural, urban, or suburban), type of program (community, university, or mixed), and accreditation of program (ACGME, AOA, or both). The other factors in this category included presence of sports medicine-trained faculty; presence of sports medicine fellowship in the institution; active promotion and encouragement of residents to go into sports medicine fellowship by program; availability of guidelines for treatment of common sports injuries; and workshops and procedure clinics specific for treating sports injuries. The third category contained questions pertaining to residents’ general interest level in sports medicine, participation in competitive sports (current or in the past), and plans to incorporate sports medicine in future practice.
Mean, standard deviations, and a chi-square test were implemented in calculating P-values.
Data was analyzed with the help of Penn State Milton S Hershey Medical Center’s Statistics Department using the Statistical Analysis System (SAS Institute Inc., Cary, NC, USA) version 9.3.
The study was approved by Penn State Milton S Hershey Medical Center’s institutional review board with study number 43220EM.
Results
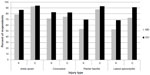
A total of 557 residents responded to the survey. Higher percentages of doctor of osteopathy (DO) residents identified the most common sports injuries – ie, ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis – as commonly occurring, compared to doctor of medicine (MD) residents (P=0.02, 0.01, <0.01, and <0.01 for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis, respectively). DO residents also appear to feel more comfortable treating these injuries compared to their MD counterparts (P=0.52, 0.04, 0.05, and <0.01 for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis, respectively) (Figure 1).
More residents from programs with sports medicine fellowships (84%, 79%, 60%, and 64%, respectively) were able to identify ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis as common injuries, and expressed comfort in treating them (94%, 80%, 93%, and 85%, respectively) compared to residents from programs with no associated sports medicine fellowship programs (81%, 75%, 58%, and 58% for identification knowledge and 93%, 76%, 89%, and 79% for treatment comfort for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis respectively). AOA-accredited programs had higher percentages of residents identifying injuries as common, as well as expressing comfort in treating them, although no statistically significant differences were observed when compared to ACGME or mixed programs, except for in relation to lateral epicondylitis (P=0.03 and <0.01 for knowledge and comfort level, respectively). Residency programs that actively promoted sports medicine fellowships had higher percentages of residents who identified sports injuries as common, as well as those who expressed comfort in treating them. Although the above factors appeared to influence residents’ knowledge of identifying the four injuries as common, other factors that affected their training appeared not to (Table 1).
In addition to the identification and comfort level in treatment of four common injuries based on medical training and practices, residents were asked to choose the correct answer for the treatment of a mallet finger and the correct definition of comminuted fracture. For these questions, more DOs correctly identified the definition of comminuted fractures (P<0.01) as well as the right treatment for a mallet finger when compared to MDs (72% DOs versus 66% MDs). Additionally, higher percentages of residents who had seen more injuries answered the two questions correctly. AOA-accredited programs and programs that actively promoted sports medicine fellowships had higher numbers of residents who accurately answered the two questions compared to ACGME- and mixed-accreditation programs and programs that did not promote sports medicine fellowships.
Other factors that did not appear to affect these two questions included region of the United States where a residency is located, type of residency program (university, community, mixed), area where residency is located (urban, suburban, rural), socioeconomic background of the patient population, presence of readily available guidelines for treating common sports injuries, availability of sports-injuries-specific clinics in residency, and presence of sports-medicine-trained faculty in the residency institution.
Residents’ attitudes towards sports medicine were measured against their propensity to identify the four common injuries as well as against their comfort level in treating them.
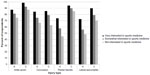
An interest in sports medicine strongly correlated with the residents identifying common sports injuries, as well as their comfort level in treating them (P=0.02, <0.01,<0.01, and <0.01 for identification knowledge and P<0.01, <0.01, 0.09, and <0.01 for treatment comfort level for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis, respectively) (Figure 2). More residents who participated in competitive sports identified more injuries as common, compared to those who did not (P<0.01, 0.01, 0.03, and 0.09 for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis, respectively). A higher percentage of residents who participated in sports were comfortable in treating these injuries, with the number comfortable in ankle sprain management being statistically significant (P=0.01).
Residents who planned on incorporating sports medicine into their future practices identified more injuries as common, compared to those who did not (P=0.03, <0.01, <0.01, and <0.01 for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis, respectively). These residents were also more comfortable in treating these injuries (P=0.05, <0.01, <0.17, and <0.01 for ankle sprain, concussion, plantar fasciitis, and lateral epicondylitis respectively).
A similar pattern was observed when residents were asked about the treatment of mallet finger and the definition of a comminuted fracture. Residents who participated in sports were more likely to choose the correct answer for treatment of mallet finger, and correctly define a comminuted fracture, with a statistically significant difference in the treatment of mallet finger question (P=0.0008). The majority of residents who had a high interest in sports medicine correctly answered the question of treatment for mallet finger (P=0.0047) and gave the correct definition of comminuted fracture (P=0.31). A higher percentage of residents who planned on incorporating sports medicine into their future practices correctly answered treatment for mallet finger (73%) and definition of comminuted fracture (78%), compared to those who did not have such a plan (61% for treatment of mallet finger and 72% definition of comminuted fracture). There was also a statistically significant difference in answering the treatment of mallet finger question (P=0.0020).
Demographical analysis revealed some expected outcomes. The more advanced a resident’s training was, the more likely he/she would identify sports injuries as common; the comfort level in treating such injuries also increased.
Sex had no statistically significant influence on knowledge of residents in identifying sports injuries as common, or on their comfort level in treating such injuries.
As residents’ training advanced, the more likely they were to correctly answer the treatment question for mallet finger and define a comminuted fracture. Half of the residents surveyed (50%) felt that 4 weeks of sports medicine rotation was appropriate for training in residency; 94% of residents thought that a family physician should be able to practice sports medicine in the office and also treat common injuries in the office (99%). Most (67%) felt one did not need sports medicine fellowship training in order to be able to do this.
Discussion
Residency education is expected to naturally influence the knowledge and practices of physicians once they are out of residency. In the United States, residency programs are either ACGME- or AOA-accredited; some programs are combined. Residents who go into an AOA-accredited residency program would have graduated from a DO medical school. In this study, DO degree holders and residents in AOA-accredited programs appeared to be more knowledgeable in identifying common sports injuries and more comfortable in treating them. The one apparent difference between the training of DO and MD physicians is osteopathic manipulation treatment, which is taught in osteopathic schools of medicine and residency, but not in allopathic schools. Osteopathic physicians are trained to “expertly evaluate the neuromusculoskeletal system through the use of manual manipulation”.12 The bones and muscles are the main focus of osteopathic manipulation treatment,13 which might account for their seemingly greater knowledge of and comfort level with sports medicine.
In the current study, the presence of sports medicine fellowship in the residency institution appeared to influence residents’ knowledge in identifying common sports injuries as well as their treatment comfort level. It is uncertain why this is the case, but having a fellowship program on site might offer residents the opportunities that fellows experience, such as game coverage or sports physicals, which in turn might provide them greater exposure to managing such injuries. However, the presence of a sports medicine faculty in a residency program did not appear to affect knowledge or treatment comfort. While the mere presence of a faculty did not appear to affect these factors, residency programs that actively promoted a sports medicine fellowship had higher percentages of residents who identified the injuries as common and were more comfortable treating them. The availability of guidelines for treating injuries and the number of injuries residents had been exposed to affected their knowledge and comfort level with the treatment of the common sports injuries presented in this study. This may be because the more a resident was exposed to such injuries, the more he or she learned from them and felt confident in managing them. The aspects of residency training that had no influence in residents’ knowledge and comfort level in treatment of common sports injuries included the type of residency program (university, community, or mixed), the area where residency is located (urban, suburban, or rural), the socioeconomic background of the patient population, and the region of the United States where a residency was located. One exception was that residents in the Midwest identified more injuries as common compared to their colleagues in other parts of the United States. It can be inferred from these results that the availability or absence of certain specialties did not have an influence on the residents. For example, a rural community will be expected to have fewer orthopedic surgeons; as such, family physicians are expected to treat a greater number of the common sports injuries, and therefore be more comfortable treating them. However, the results of this study did not support this.
Residents’ attitudes towards sports medicine appeared to have an impact on their identification of sports injuries as common and on their comfort level in treating those injuries. A strong interest in sports medicine strongly correlated with residents identifying sports injuries as common, as well as increased comfort in treating them, with statistically significant differences. Residents who participated in competitive sports also identified more injuries as common and perceived themselves to be more comfortable in treating them compared to those who did not. Thus, it can be deduced from these results that residents with a strong interest in sports medicine might be participating in activities that increase their knowledge in this field. These activities could include following trends in sports medicine (reading published articles), covering sports events, or following sports in general. For residents who had participated in sports, the chances that they or teammates had been exposed to these injuries might be very high, and they could have gained greater knowledge from those experiences. Having been patients themselves might have made them aware of how these injuries are treated, perhaps even improving their comfort level in treating them. Residents who planned on incorporating sports medicine into their future practices identified more injuries as common compared to those who did not, with statistically significant differences, and they were more comfortable treating those injuries as well. It stands to reason that residents who are considering practicing sports medicine would be inclined to learn more about what they would be doing in the future compared to residents who are interested in other fields.
Regarding the residents’ views on current sports medicine training and future practice, many residents felt family physicians should be able treat common sports injuries and practice sports medicine in the office without having been through sports medicine fellowship training. Over 95% of the residents felt that 4 or more weeks’ rotation in sports medicine was sufficient to learn how to treat such common injuries. Previous studies in pediatric and internal medicine residents focused on whether residents are comfortable in treating these injuries. This study expands on identifying why this is the case in family medicine residents. A limitation of this study is exclusion of military family medicine residency programs who are not allowed to complete studies that are not sanctioned by the military. An additional limitation is our inability to calculate an accurate rate of response. This is due to the fact that we are not aware of how many residents actually received the survey link since it was sent through their program directors and coordinators. This can also affect the response rate as not all directors or coordinators will forward emails to residents.
Conclusion
Several factors shape the training of a family medicine resident. This study pointed out factors that affect a family medicine resident’s ability to identify a common sports injury as well as his or her comfort level in treating these injuries. A resident’s medical background coupled with the residency program’s efforts toward sports medicine, such as active promotion of fellowship, may significantly impact knowledge and comfort level in treating common sports injuries. The availability of specific guidelines for treating some of the common injuries could increase residents’ awareness about common sports injuries and enhance their comfort level in treating these injuries. Residents’ attitudes towards sports medicine could also have an impact on their knowledge and treatment comfort level. Future studies should focus on accessing current practicing family physicians’ treatment comfort level and knowledge regarding common sports injuries as several years in practice may make up for loss experience in residency or medical school.
Acknowledgments
The authors would like to thank Erik B. Lehman – Penn State Milton S. Hershey Medical Center Statistics Department. This paper was presented at: Society of Teachers of Family Medicine Annual Spring Conference, May 3–7, 2014, San Antonio, TX, USA; and American Medical Society of Sports Medicine Annual Conference, April 4–9, 2014, New Orleans, LA, USA.
Disclosure
The authors report no conflicts of interest in this work.
References
Stirling JM, Landry GL. Sports medicine training during pediatric residency. Arch Pediatr Adolesc Med. 1996;150(2):211–215. | |
Adirim TA, Cheng TL. Overview of injuries in the young athlete. Sports Med. 2003;33(1):75–81 | |
CDC. National estimates of nonfatal injuries treated in hospital emergency departments—United States, 2000. MMWR. 2001;50(17):340–46. | |
Hambidge SJ, Davidson AJ, Gonzalez R, Steiner JF. Epidemiology of pediatric injury-related primary care office visits in the United States. Pediatrics. 2002;109(4):559–565. | |
Matzkin E, Smith EL, Freccero D, Richardson AB. Adequacy of education in musculoskeletal medicine. J Bone Joint Surg Am. 2005;87(2):310–314. | |
Bucholtz JR, Matheny SC, Pugno PA, David A, Bliss EB, Korin EC. Task force report 2. Report of the task force on medical education. Ann Fam Med. 2004;2(Suppl 1):S51–S64. | |
Duane M, Green LA, Dovey SM, Lai S, Graham R, Fryer GE. Length and content of family practice residency training. J Am Board Fam Pract. 2002;15(3):201–208. | |
Lebensohn P, Campos-Outcalt D, Senf J, Pugno PA. Experience with an optional 4-year residency: The university of Arizona family medicine residency. Fam Med. 2007;39(7):488–494. | |
Smits AK, Walsh E, Ross RG, Gillanders WR, Saultz JW. Residency applicants’ perspectives on family medicine residency training length. Fam Med. 2006;38(3):172–176. | |
Sweeney CL, Davidson M, Melgar T, Patel D, Cucos D. The current status of sports medicine training in United States internal medicine residency programmes. Br J Sports Med. 2003;37(3):219–225. | |
Demorest RA, Bernhardt DT, Best TM, Landry GL. Pediatric residency education: Is sports medicine getting its fair share? Pediatrics. 2005;115(1):28–33. | |
DiGiovanna EL, Schiowitz S, Dowling DJ, editors. An Osteopathic Approach to Diagnosis and Treatment, Third Edition. Philadelphia, PA: Lippincott Williams and Wilkins; 2005. | |
Lesho EP. An overview of osteopathic medicine. Arch Fam Med. 1999;8(6):477–484. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.