Back to Journals » OncoTargets and Therapy » Volume 8
Expressions and clinical significance of autophagy-related markers Beclin1, LC3, and EGFR in human cervical squamous cell carcinoma
Authors Hu Y, Lei X, Zhang H, Ma J, Yang W, Chen M, Cui J, Zhao H
Received 18 April 2015
Accepted for publication 16 June 2015
Published 24 August 2015 Volume 2015:8 Pages 2243—2249
DOI https://doi.org/10.2147/OTT.S86844
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Daniele Santini
Yun-Feng Hu,1 Xia Lei,2 Hong-Yi Zhang,3 Jun-wei Ma,1 Wei-wei Yang,1 Min-lin Chen,1 Jie Cui,1,4 Hong Zhao1
1Department of Oncology, 2Department of Gynecology, 3Department of Urology, Yan’an University Affiliated Hospital, Yan’an, Shaanxi Province, People’s Republic of China; 4Department of Oncology, the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi Province, People’s Republic of China
Purpose: We aimed to investigate the expression of EGFR and the autophagy-related markers Beclin1 and LC3 in cervical cancer.
Methods: Beclin1, LC3, and EGFR expression were analyzed in 80 samples of cervical squamous cell carcinoma (SCC), 40 samples of high-grade cervical intraepithelial neoplasia (CIN), and 40 samples of normal cervical tissues by immunohistochemistry. The protein expression rates were analyzed with χ2 and Fisher’s exact tests. Differences in overall survival (OS) were determined using the Kaplan–Meier method and log-rank tests.
Results: Cervical cancer, high-grade CIN, and normal cervical epithelial cells expressed Beclin1 in 26.2%, 77.5%, and 82.5% of patients, respectively, and expressed LC3 in 28.8%, 70.0%, and 75.0% of patients, respectively. There was a significant difference between cervical SCC and high-grade CIN or normal cervical epithelial cells (P=0.000). Cervical cancer cells, high-grade CIN cells, and normal cervical epithelial cells expressed EGFR in 68.8%, 62.5%, and 12.5% of patients, respectively. There was a significant difference between cervical SCC or high-grade CIN and normal cervical epithelial cells (P=0.000). No significant association between Beclin1 or LC3 or EGFR expression and various clinicopathological parameters was observed in cervical SCC. There was no significant correlation between Beclin1, LC3, EGFR expression, and 5-year OS rates of cervical SCC patients. Beclin1- or LC3-negativity with EGFR-positivity in cervical SCC was associated with a higher Federation International of Gynecology and Obstetrics (FIGO) stage (P=0.011 and P=0.013, respectively) and pelvic lymph node metastasis (P=0.036 and P=0.092, respectively). The 5-year OS rates did not significantly differ between Beclin1- or LC3-positive and -negative patients with positive EGFR.
Conclusion: Autophagy was downregulated and EGFR was upregulated in cervical SCC. Autophagy downregulation combined with EGFR upregulation promotes the progression of cervical SCC.
Keywords: autophagy, Beclin1, LC3, EGFR, cervical squamous cell carcinoma, immunohistochemistry
Introduction
Cervical cancer is one of the most common causes of morbidity and mortality due to gynecologic malignancies worldwide.1 Histopathologically, the most common subtype of cervical cancer is squamous cell carcinoma (SCC), which accounts for up to 80% of these tumors.2 Poor prognostic factors for early-stage cervical cancer include large tumor diameter, pelvic lymph node metastasis, parametrial invasion, positive surgical margins, and deep stromal and lymphovascular invasion.3 However, whether such prognostic factors are sufficiently accurate to estimate prognosis and determine therapeutic strategies remains controversial. Thus, biological characteristics of cervical cancer should be understood, and novel molecular markers should be identified to accurately predict the prognosis of patients.
Autophagy is a process of self-digestion in which redundant organelles and long-lived proteins are removed to provide a survival mechanism for cells under stress, such as hypoxia and starvation.4 Autophagy has biphasic function in cancer development. Autophagy suppresses the initiation of tumors by clearing damaged organelles, maintaining cell homeostasis and protecting normal cell growth. On the contrary, in the development of cancer, when tumor cells are subjected to stressful conditions, autophagy is upregulated to maintain metabolic homeostasis and cell survival, through reduced growth and increased catabolic lysis of excess or unnecessary proteins and organelles. The Beclin1 and cytosolic LC3 genes play an important role in mammalian autophagy, both of which are involved in autophagosome formation.5–8
EGFR is an oncogenic receptor tyrosine kinase, which is hyperactive in various types of solid tumors.9 EGFR is implicated in cellular proliferation, metastasis, angiogenesis, apoptosis inhibition, chemoresistance, and radioresistance. EGFR activation regulates autophagy, through multiple signaling pathways.10 In this study, the expression of EGFR and the autophagy-related markers Beclin1 and LC3 in cervical SCC, high-grade cervical intraepithelial neoplasia (CIN), and in normal cervical epithelial tissues was investigated. The prognostic significance of EGFR and Beclin1 and LC3 expression in cervical SCC was also evaluated.
Materials and methods
Patients and specimen selection
Paraffin-embedded pathological specimens were obtained from the archives of the Department of Pathology of Yan’an University Affiliated Hospital (People’s Republic of China) between January 2007 and January 2009. A total of 80 tumor samples with Federation International of Gynecology and Obstetrics (FIGO) stage I–II cervical SCC were obtained from radical surgery. In addition, 40 samples with high-grade CIN obtained from conization of the cervix and 40 samples with normal cervical epithelial tissues obtained from surgery for myoma of the uterus were included in this study. Approval for the current project was obtained from the local ethics committee, together with written informed consent from each patient. The patients were aged 28–70 years (median, 45 years). Twenty cervical SCC patients with pelvic lymph node metastasis accepted platinum-based concurrent chemoradiotherapy.
Immunohistochemical staining of Beclin1, LC3, and EGFR
Paraffin-embedded histological specimens of 80 cervical SCC tissue samples, 40 high-grade CIN tissue samples, and 40 normal cervical tissues samples were sectioned (thickness 5 μm). Beclin1, LC3, and EGFR expression levels were analyzed by immunohistochemical staining. The primary detection antibodies, anti-Beclin1 antibody (Abcam, Cambridge, UK), anti-LC3B (Abcam), and anti-EGFR (Bioworld Technology, St Louis Park, MN, USA), were used at a dilution of 1:200. The sections were deparaffinized, dehydrated, and washed three times with phosphate-buffered saline (PBS) (5 minutes per process) before endogenous peroxidase activity was blocked by incubation with 3% hydrogen peroxide solution. The specimens were then washed with PBS. Nonspecific binding was blocked by incubating the slides with normal goat serum for 15 minutes at 37°C and then with primary detection antibodies overnight at 4°C. The slides were washed three times with PBS and incubated with anti-rabbit and -mouse secondary antibody (Boster, Wuhan, People’s Republic of China) at 37°C for 40 minutes. Subsequently, the slides were washed again three times with PBS and incubated with diaminobenzidine (Boster) for 10 minutes to visualize immunolabeling.
Assessment of Beclin1, LC3, and EGFR expression
All slides were evaluated independently by two experienced pathologists. Beclin1, LC3, and EGFR expression were semiquantitatively scored according to staining intensity and the percentage of stained cells. At least five of the largest immunostained areas for each antibody were selected. Staining intensity was defined as follows: negative (0), weak (1+), moderate (2+), and strong (3+). The percentage of immunoreactive tumor cells was rated as follows: no staining (0), <30% (1), and >30% (2). To obtain the grade of the scored expression, the percentage of immunoreactive tumor cells was multiplied by staining intensity; the scoring pattern was defined as follows: negative (0–1), low positive (2–4), or high positive (5–6).11
Statistical analysis
All data were analyzed using SPSS, version 19.0 (IBM Corp., Armonk, NY, USA). The χ2 and Fisher’s exact tests were used to compare different protein expression levels. Overall survival (OS) time was defined from the day of surgery to the day of death or last follow-up visit. The Kaplan–Meier method and log-rank tests were used to evaluate differences in OS rates. P<0.05 was considered to indicate statistical significance.
Results
Expression of Beclin1, LC3, and EGFR in cervical SCC, high-grade CIN, and normal cervical epithelial tissues
Immunohistochemical analysis showed that Beclin1 and LC3 were predominantly expressed in the cytoplasm of cells. Cervical cancer cells, high-grade CIN cells, and normal cervical epithelial cells expressed Beclin1 in 26.2% (21/80), 77.5% (31/40), and 82.5% (33/40) of patients, respectively, and expressed LC3 in 28.8% (23/80), 70.0% (28/40), and 75.0% (30/40) of patients, respectively. There was a significant difference between cervical SCC and high-grade CIN or normal cervical epithelial cells (P=0.000).
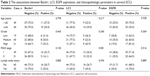
Specific EGFR staining was observed mainly in the cytoplasm or cell membrane. Cervical cancer cells, high-grade CIN cells, and normal cervical epithelial cells expressed EGFR in 68.8% (55/80), 62.5% (25/40), and 12.5% (5/40) of patients, respectively (Table 1; Figure 1). There was a significant difference between cervical SCC or high-grade CIN and normal cervical epithelial cells (P=0.000) (Table 1; Figure 1).
Clinicopathological significance of Beclin1, LC3, and EGFR in cervical SCC
The associations between the expression of Beclin1, LC3, and EGFR and clinicopathological parameters, including age, FIGO stage, pathological differentiation, and pelvic lymph node metastasis in 80 patients with cervical SCC were analyzed. No significant association between Beclin1 or LC3 or EGFR expression and various clinicopathological parameters (P>0.05) was observed (Table 2).
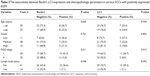
The associations between the expression of Beclin1, LC3, and the clinicopathological parameters of 55 EGFR-positive cervical SCC patients were analyzed. Beclin1- or LC3-negativity with EGFR-positivity was associated with higher FIGO stage (P=0.011 and P=0.013, respectively) and pelvic lymph node metastasis (P=0.036 and P=0.092, respectively) (Table 3).
Correlation between Beclin1, LC3, or EGFR expression and overall survival of patients with cervical SCC
The average duration of follow up was 63.5 months (range 8–79 months). The 5-year OS rates of Beclin1-negative and -positive patients were 71.2% and 85.7%, respectively (χ2=1.69, P=0.194) (Figure 2A). The 5-year OS rates of LC3-negative and -positive patients were 71.9% and 82.6%, respectively (χ2=0.889, P=0.346) (Figure 2B). The 5-year OS rates of EGFR-negative and -positive patients were 88.0% and 69.1%, respectively (χ2=3.182, P=0.074) (Figure 2C). The 5-year OS rates of Beclin1-negative and -positive patients with positive EGFR were 64.1% and 81.3%, respectively (χ2=1.482, P=0.224) (Figure 2D). The 5-year OS rates of LC3-positive and -negative patients with positive EGFR were 64.3% and 84.6%, respectively (χ2=1.693, P=0.193) (Figure 2E).
Discussion
In this study, Beclin1 and LC3 expression was significantly decreased in cervical SCC compared with that in high-grade CIN and normal cervical epithelial tissues. This result is similar to that described in other studies in which the expression levels of both Beclin1 and LC3 were significantly lower in cervical SCC cells than in normal squamous epithelial cells.12 Other studies have also demonstrated that Beclin1 or LC3 expression is frequently decreased in tumor cells, such as breast cancer, hepatocellular carcinoma, and lung cancer, compared with that in normal cells.13–15 Beclin1 and LC3 genes play a crucial role in mammalian autophagy. Beclin1 is involved in the signaling pathway that activates autophagy and in the initial step of autophagosome formation. In vivo studies have further revealed that defective autophagy, such as in Beclin1 knockdown, provides an oncogenic stimulus, causing malignant transformation and spontaneous tumors.16 LC3 comprises a soluble LC3I and a lapidated form called LC3II. LC3II is recruited into autophagosomes, which are considered to be a reliable marker of autophagy.5 On the basis of these results, we propose that protective autophagy is inhibited in cervical SCC, and this condition may be related to carcinogenesis. However, other studies have shown that autophagy is upregulated in tumors, including gastrointestinal cancers, pancreatic cancer, and gallbladder cancer.17–19 This finding may be explained by the biphasic function of autophagy in cancer development. On the one hand, autophagy is considered to be a tumor-suppressive mechanism by which damaged organelles are eradicated, thereby maintaining cell homeostasis by protecting normal cell growth or inducing caspase-independent autophagic cell death. On the other hand, autophagy represents a key survival mechanism in which tumor cells respond to microenvironmental stress during cancer development.
The present study showed Beclin1 and LC3 expression was not significantly correlated with clinicopathological parameters, including age, FIGO stage, pathologic differentiation, and pelvic lymph node metastasis in patients with cervical SCC. Furthermore, there were no significant differences in the 5-year OS rate between the Beclin1- or LC3-positive and -negative groups. These results are similar to those obtained in a previous study, which showed that Beclin1 and LC3 expression in 50 cases of FIGO stage I–II cervical SCC were not significantly associated with age, FIGO stage, pathologic differentiation, or pelvic lymph node metastasis. However, the high Beclin1 expression group exhibited a significantly higher 3-year OS rate than did the low Beclin1 expression group.2 In another study, Beclin1 and LC3 expression were also found to be not significantly associated with various clinicopathological characteristics in cervical SCC, including tumor tissue obtained from 56 tumor, node, metastasis (TNM) stage I–II patients and 24 stages III–IV patients. However, high clinical TNM stage and lymph node metastasis have been identified in Beclin1- and LC3-negative patients with positive high-risk human papillomavirus (HPV) infection.20 Similar results have been observed in other cancer types. For instance, Jiang et al found that Beclin1 and LC3 expression were not associated with the age, sex, smoking, histological type, lymph node metastasis, or TNM stage of lung cancer patients.15 Yoshioka et al revealed that LC3 expression was not correlated with various clinicopathological factors and survival in gastrointestinal cancer.17 Conversely, other studies have revealed that Beclin1 or LC3 expression exhibits significant negative correlations with cancer differentiation, lymph node metastasis, and prognosis of cervical cancer12 as well as pancreatic cancer,18 gastric carcinoma,21 esophageal SCC,22 and hepatocellular carcinoma.23 These contradictory findings may be explained in two ways. First, autophagy is implicated in different functions in diverse tumors and different phases of tumor development. For instance, autophagy may suppress tumorigenesis in the early phase of tumor development. However, autophagy may be a key tumor cell survival mechanism in response to microenvironmental stress in the late phase of tumor development. Second, the small number of cancer tissue samples included in the present may limit the interpretation of our results. Therefore, large-sample studies should be conducted to confirm the role of autophagy in cervical SCC.
Similarly, the present study showed that EGFR expression was not significantly correlated with clinicopathological parameters. Furthermore, there was no significant difference in 5-year OS rate between the EGFR-positive and -negative groups. We further investigated the clinicopathological significance of Beclin1 or LC3 expression in EGFR-positive cervical SCC. The results revealed that the Beclin1- or LC3-negativity with EGFR-positivity was associated with higher FIGO stage (P=0.011 and P=0.013, respectively) and pelvic lymph node metastasis (P=0.036 and P=0.092, respectively). This study also revealed that the 5-year OS rate of Beclin1- or LC3-negative patients with positive EGFR decreased compared with those of Beclin1- or LC3-positive patients with positive EGFR. However, no significant difference was observed between the two groups, which may have been due to the small number of cases and short follow-up duration. All of the patients who died were found with stage II or pelvic lymph node metastasis. On the basis of these results, we propose that the downregulation of autophagy or the upregulation of EGFR alone is insufficient to accelerate the progression of cervical SCC. Conversely, the downregulation of autophagy combined with the upregulation of EGFR may promote the rapid progression of cervical SCC. Autophagy downregulation leads to tumorigenesis in the early phase of tumor development. Simultaneously, EGFR upregulation triggers downstream signaling cascades through the binding of growth factors; thus, cancer cell proliferation and survival are enhanced. Indeed, the interaction of these two factors may lead to the initiation and progression of cervical SCC. Therefore, EGFR blockers combined with autophagy inducers may be a good strategy for the management of cervical SCC.
Acknowledgments
We would like to offer special thanks to the Department of Pathology of Yan’an University Affiliated Hospital for their help with the manuscript. The study was supported by the Scientific and Technological Project Project of Yan’an (grant number 2013-kw22).
Disclosure
The authors report no conflicts of interest in this work.
References
Benard VB, Thomas CC, King J, Massetti GM, Doria-Rose VP, Saraiya M; Centers for Disease Control and Prevention (CDC). Vital signs: cervical cancer incidence, mortality, and screening – United States, 2007–2012. MMWR Morb Mortal Wkly Rep. 2014;63(44):1004–1009. | ||
Lorin L, Bertaut A, Hudry D, et al. About invasive cervical cancer: a French population based study between 1998 and 2010. Eur J Obstet Gynecol Reprod Biol. 2015;191:1–6. | ||
Zhu W, Pan X, Li F, Zhang Y, Lu X. Expression of Beclin 1 and LC3 in FIGO stage I–II cervical squamous cell carcinoma and relationship to survival. Tumour Biol. 2012;33(5):1653–1659. | ||
De Duve C, Wattiaux R. Functions of lysosomes. Annu Rev Physiol. 1966;28:435–492. | ||
Kimmelman AC. The dynamic nature of autophagy in cancer. Genes Dev. 2011;25(19):1999–2010. | ||
Shimizu S, Kanaseki T, Mizushima N, et al. Role of Bcl-2 family proteins in a non-apoptotic programmed cell death dependent on autophagy genes. Nat Cell Biol. 2004;6(12):1221–1228. | ||
Yu L, Alva A, Su H, et al. Regulation of an ATG7-beclin 1 program of autophagic cell death by caspase-8. Science. 2004;304(5676):1500–1502. | ||
Kubisch J, Türei D, Földvári-Nagy L, et al. Complex regulation of autophagy in cancer – integrated approaches to discover the networks that hold a double-edged sword. Semin Cancer Biol. 2013;23(4):252–261. | ||
Khalil MY, Grandis JR, Shin DM. Targeting epidermal growth factor receptor: novel therapeutics in the management of cancer. Expert Rev Anticancer Ther. 2003;3(3):367–380. | ||
Cui J, Hu YF, Feng XM, et al. EGFR inhibitors and autophagy in cancer treatment. Tumour Biol. 2014;35(12):11701–11709. | ||
Choi J, Jung W, Koo JS. Expression of autophagy-related markers beclin-1, light chain 3A, light chain 3B and p62 according to the molecular subtype of breast cancer. Histopathology. 2013;62(2):275–286. | ||
Cheng HY, Zhang YN, Wu QL, Sun XM, Sun JR, Huang X. Expression of beclin 1, an autophagy-related protein, in human cervical carcinoma and its clinical significance. Eur J Gynaecol Oncol. 2012;33(1):15–20. | ||
Zarzynska JM. The importance of autophagy regulation in breast cancer development and treatment. Biomed Res Int. 2014;2014:710345. | ||
Ding ZB, Shi YH, Zhou J, et al. Association of autophagy defect with a malignant phenotype and poor prognosis of hepatocellular carcinoma. Cancer Res. 2008;68(22):9167–9175. | ||
Jiang ZF, Shao LJ, Wang WM, Yan XB, Liu RY. Decreased expression of Beclin-1 and LC3 in human lung cancer. Mol Biol Rep. 2012;39(1):259–267. | ||
Dalby KN, Tekedereli I, Lopez-Berestein G, Ozpolat B. Targeting the prodeath and prosurvival functions of autophagy as novel therapeutic strategies in cancer. Autophagy. 2010;6(3):322–329. | ||
Yoshioka A, Miyata H, Doki Y, et al. LC3, an autophagosome marker, is highly expressed in gastrointestinal cancers. Int J Oncol. 2008;33(3):461–468. | ||
Fujii S, Mitsunaga S, Yamazaki M, et al. Autophagy is activated in pancreatic cancer cells and correlates with poor patient outcome. Cancer Sci. 2008;99(9):1813–1819. | ||
Park JY, Kim HS, Cho H, et al. Clinicopathologic correlation of autophagy-related Beclin-1 expression in gallbladder cancer. Hepatogastroenterology. 2014;61(134):1494–1500. | ||
Wang HY, Yang GF, Huang YH, et al. Reduced expression of autophagy markers correlates with high-risk human papillomavirus infection in human cervical squamous cell carcinoma. Oncol Lett. 2014;8(4):1492–1498. | ||
Chen YB, Hou JH, Feng XY, et al. Decreased expression of Beclin 1 correlates with a metastatic phenotypic feature and adverse prognosis of gastric carcinomas. J Surg Oncol. 2012;105(6):542–547. | ||
Chen Y, Lu Y, Lu C, Zhang L. Beclin-1 expression is a predictor of clinical outcome in patients with esophageal squamous cell carcinoma and correlated to hypoxia-inducible factor (HIF)-1alpha expression. Pathol Oncol Res. 2009;15(3):487–493. | ||
Osman NA, Abd El-Rehim DM, Kamal IM. Defective Beclin-1 and elevated hypoxia-inducible factor (HIF)-1α expression are closely linked to tumorigenesis, differentiation, and progression of hepatocellular carcinoma. Tumour Biol. Epub 2015 Jan 17. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.