Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Evaluating depressive symptoms in mania: a naturalistic study of patients with bipolar disorder
Authors Young A , Eberhard J
Received 11 February 2015
Accepted for publication 10 March 2015
Published 29 April 2015 Volume 2015:11 Pages 1137—1143
DOI https://doi.org/10.2147/NDT.S82532
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Editor who approved publication: Dr Roger Pinder
Allan H Young,1 Jonas Eberhard1,2
1Institute of Psychiatry, King’s College London, London, UK; 2Corporate Medical Affairs, H. Lundbeck A/S, Copenhagen, Denmark
Objective: This study aimed to evaluate patients with bipolar I disorder (BD-I) who have mania with depressive symptoms and who meet the new “with mixed features” specifier of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5).
Method: This prospective, multinational, naturalistic study surveyed psychiatrists and their patients with BD-I from October 2013 to March 2014. Eligible patients had BD-I, had a (current) manic episode, and had experienced onset of a manic episode within the previous 3 months. Psychiatrists provided patient information on depressive symptoms (DSM-5 criteria); symptoms of anxiety, irritability, and agitation; suicide attempts; and physician satisfaction with treatment response. Data were stratified according to whether patients met the criteria for the BD-I “with mixed features” specifier of DSM-5 (≥3 depressive symptoms) or not, and characteristics were compared between the two subgroups. Patients also self-reported on depressive symptoms using the Mini-International Neuropsychiatric Interview module questionnaire.
Results: Overall, 34% of 1,035 patients met the criteria for BD-I “with mixed features,” exhibiting ≥3 depressive symptoms during their current manic episode. This correlated with the matched patient self-reports of depressive symptoms. During their current manic episode, BD-I patients “with mixed features” had more severe symptoms of anxiety, irritability, and agitation (average composite severity score of 4.1 vs 3.4), a higher incidence of suicide attempts (38% vs 9%), and more physician dissatisfaction with treatment response (22% vs 14%), compared to patients with 0–2 depressive symptoms (all P<0.05).
Conclusion: This study found that patients with BD-I “with mixed features” (ie, ≥3 depressive symptoms during a manic episode), suffered, on average, from a greater burden of disease than patients with pure mania. Improved identification of these patients may help to optimize treatment outcomes.
Keywords: bipolar disorder, mania with depressive symptoms, mixed features, DSM-5
Introduction
Bipolar I disorder (BD-I) is a chronic disease that has a lifetime prevalence of approximately 1% and is characterized by periods of mania, depression, or combinations of both (mixed states).1–3 Manic episodes with depressive symptoms are generally more severe and are associated with a poorer prognosis, than pure manic episodes.4,5 However, although these types of mixed episodes are common – occurring in at least 30% of patients with BD5–7 – they are not easily or consistently identified by clinicians.4,5 Reaching a correct diagnosis through the systematic search for depressive symptoms during a manic episode is likely to be important for optimizing patient outcomes.4
Recently, the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) provided a new “with mixed features” specifier for hypomanic, manic, or depressive episodes.8 At least three of six depressive symptoms must be present to allocate the specifier to a manic or hypomanic episode.8 To accompany this, a short, structured Mini-International Neuropsychiatric Interview (MINI) module has also been developed to gather patient input on the DSM-5 specifier.
The objectives of the current research were to assess the following:
- the number of patients presenting with depressive symptoms during a manic episode according to the DSM-5 “with mixed features” specifier;
- the association between the presence of depressive symptoms during a manic episode and the following: specific mixed symptoms (anxiety, irritability, and agitation); suicidality; physician satisfaction with treatment; and depressive symptoms assessed in the MINI module.
Methods
Study design
This prospective, naturalistic study aimed to evaluate patients with BD-I who present with mania and depressive symptoms.
The study surveyed psychiatrists and patients from centers in Australia, Brazil, Canada, Germany, Italy, Spain, Turkey, and the UK. The study began in October 2013, with the final data collected on March 31, 2014.
The study was conducted in compliance with the relevant codes of conduct (European Pharmaceutical Market Research Association [EphMRA]; Association of the British Pharmaceutical Industry [ABPI]). Patient data were anonymized, stored, and processed in agreement with the requirements of the EU Data Protection Directive 95/46/EC.
Study populations
On the basis of a representative mix of in-/outpatient settings and regions for each country, psychiatrists who were treating patients with BD-I were invited to take part in the study. Physicians eligible for study inclusion were required to be actively managing and treating adult patients diagnosed with BD-I (refer criteria below); to have been qualified for a period ranging between 3 years and 30 years (between 2 years and 38 years in Australia); and to have a patient caseload comprising ≥20 patients with BD-I per month (≥14 patients/month in Australia) and ≥8 patients with both BD-I and a manic episode per month (≥3 patients/month in Australia; ≥5 patients/month in Germany and the UK).
Patients’ eligibility criteria were as follows: age ≥18 years; diagnosis of BD-I (DSM-IV-TR [DSM-IV-text revision] criteria); experiencing a (current) manic episode with onset within the last 3 months; and a clinical condition compatible with reliably completing a short questionnaire (according to investigator judgment).
Data collection
Each psychiatrist completed an online survey for up to six consecutively consulted patients with BD-I who had a (current) manic episode. The survey assessments included the following: presence of depressive symptoms (DSM-5 criteria; Table 1);8 Clinical Global Impression of bipolar disorder (CGI-BP);9 a global assessment of symptoms (anxiety, irritability, and agitation, with severity being rated from 1 [absent] to 7 [very severe]); frequency of suicide attempts during current manic episode and over lifetime; and physician satisfaction with treatment response (rated from 1 to 7, with ratings 1–3= dissatisfied, 4= neither satisfied nor dissatisfied; 5–7= satisfied). Patient demographics and disease history were also recorded.
Each psychiatrist also invited his or her patients to complete the recently developed and validated MINI module for the DSM-5 specifier, as a paper questionnaire. The MINI module comprises nine questions about the presence or absence of six depressive features in line with DSM-5 criteria (Table 1).10
Statistical analyses
Only matched data were included for analysis, ie, patients for whom data were available from both the physician assessment and the MINI module patient questionnaire.
Data on patient and disease characteristics were analyzed descriptively for the study population, with patients stratified according to whether they met the criteria for the BD-I “with mixed features” specifier of DSM-5. At least three of six depressive symptoms must be present to allocate the specifier:
- 0–2 depressive symptoms (did not meet the criteria for mixed features);
- ≥3 depressive symptoms (met the criteria for mixed features).
Statistical comparisons between the patient subgroups were made using a two-sided t-test, and values of P<0.05 were considered statistically significant. Data were statistically analyzed using Confirmit Horizons v17.5 software.
The study also examined the subgroup of patients with no depressive symptoms according to DSM-5 criteria for BD-I, and analyses were descriptive only – no statistical comparisons were made.
Results
Population characteristics
A total of 184 physicians (181 psychiatrists plus 3 “Nervenärzte” [= combined neurologist/psychiatrist] from Germany), with 1,035 patient reports and matching MINI module questionnaires, were eligible for inclusion (from among an initial 372 respondents and 1,355 patient records). Patients had a mean age of 40 years (range: 18 years–73 years); 52% were female; and 44% were in employment.
Physicians had a mean of 14 years’ experience, and a mean caseload of 57 patients with BD-I per month (22% of total caseload) – approximately half (51%) of whom were likely to be in a manic episode at any one time. Physicians spent most (68%) of their time working with outpatients in a hospital or office setting.
Physicians’ survey
According to physicians (CGI-BP rating), in terms of overall bipolar illness, the majority (67%, n=691) of patients were moderately to markedly ill during their current manic episode. During this latest episode, 69% (n=715) of patients experienced at least one depressive symptom, and only 31% (n=320) experienced no depressive symptoms, according to DSM-5 criteria. In total, 34% (n=348) of patients experienced ≥3 depressive symptoms and thus met the criteria for the DSM-5 specifier for BD “with mixed features.”
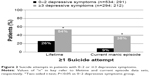
A statistically significantly higher proportion of patients with mixed features (ie, ≥3 depressive symptoms) presented with anxiety or irritability during their current manic episode, compared with patients without mixed features (ie, 0–2 depressive symptoms) (anxiety: 99% vs 78%, respectively, P<0.05; irritability: 97% vs 91%, respectively, P<0.05) (Figure 1). The between-group difference in agitation was not significant (95% vs 92%, respectively). Fifteen patients in the 0–2 depressive symptoms group experienced none of these three symptoms. The severity of anxiety, irritability, and agitation was significantly greater in patients with ≥3 depressive symptoms compared with patients with 0–2 depressive symptoms (average composite severity score of 4.1 vs 3.4; P<0.05); patients with no symptoms were scored 1 (“symptoms absent”). Patients with ≥3 depressive symptoms were also statistically significantly more likely to have made at least one suicide attempt during their lifetime and during their current manic episode, compared to those with 0–2 depressive symptoms (both P<0.05; Figure 2).
Twenty-two percent of physicians reported that they were dissatisfied with the treatment response in patients with ≥3 depressive symptoms, compared with 14% of physicians for patients with 0–2 depressive symptoms. This difference was statistically significant (P<0.05) (Figure 3).
  | Figure 3 Physician satisfaction with current treatment for patients with 0–2 or ≥3 depressive symptoms. |
Patients in the subgroup with no depressive symptoms (n=320) had less anxiety (70%), irritability (88%), and agitation (91%) than the symptom subgroups described above, with an overall severity score of 3.2. Eighteen percent of patients had made one or more suicide attempts during their lifetime, 4% doing so during their current manic episode. Only 12% of physicians were dissatisfied with the treatment response in this patient subgroup.
Patient questionnaire: MINI module
Patient responses to the nine questions of the MINI module questionnaire were consistent with the physician assessment using the DSM-5 “with mixed features” specifier. A significantly higher proportion of patients diagnosed with ≥3 depressive symptoms answered “yes” to each of the MINI module questions (38%–76% across questions) during their current manic episode, compared with patients diagnosed with 0–2 depressive symptoms (10%–27%); P<0.05 for all comparisons (Figure 4A). As may be expected, there were even fewer positive responses in the subgroup of patients diagnosed with no depressive symptoms (6%–17%).
  | Figure 4 Percentage of patients with 0–2 or ≥3 depressive symptoms who exhibited particular depressive symptoms according to (A) patient self-report (MINI module questionnaire) and (B) physician (DSM-5 criteria), ratings. |
The frequencies of individual depressive symptoms, as assessed by patients in the MINI module questionnaire, followed a pattern similar to those of the physicians’ ratings (DSM-5 criteria) (Figure 4B).
Discussion
BD-I is a dimensional disease, characterized by fluctuations between periods of mania and depression. There may also be prolonged periods when patients experience a mix of symptom types, such as mania with depressive symptoms. Mixed episodes represent a severe presentation of BD-I – patients are characterized by a greater risk of suicide, higher frequency of episodes, more rapid cycling,11 an earlier appearance of symptoms, and more comorbidities including substance-use disorders and anxiety disorders, in comparison to patients with nonmixed episodes (reviewed by Swann et al12 and Goldberg and McElroy13). Moreover, diagnosis of this complex condition can be challenging,4 and manic episodes with depressive symptoms also generally have a poorer prognosis than pure manic episodes.4,5,11,14,15
The DSM-IV-TR diagnostic criteria for BD-I provide clear distinctions between the concepts of manic, mixed, and depressive states of BD.16 However, concerns that these definitions did not reflect clinical reality led to a revision of the boundaries in the fifth edition of DSM (DSM-5), which now addresses the convergence of the two states with the less restrictive “with mixed features” specifier.8 The “with mixed features” specifier applies in episodes where syndromal or subthreshold symptoms from the opposing pole are present during a full-mood episode (ie, depressive symptoms during hypo/manic episodes and vice versa).8 As listed in Table 1, the DSM-5 proposes a minimum of three of six depressive symptoms for the mixed specifier to be applied to a manic episode.8
Applying this new DSM-5 specifier in a naturalistic setting, the current study evaluated patients with BD-I and depressive symptoms in mania. On the basis of a large psychiatrist-based patient population across eight countries, the study found that one third of patients with BD-I presented with ≥3 depressive symptoms during their current manic episode and thus met the criteria for the DSM-5 specifier for BD “with mixed features.” In line with previous findings,4,5,12,13 psychiatrists reported that these patients had, on average, a greater burden of disease; experienced more severe anxiety, irritability, and agitation; and had a higher incidence of suicide attempts, both during their lifetime and during their current manic episode, compared with patients who did not meet the criteria for mixed features (ie, 0–2 depressive symptoms).
The high frequency and severity of anxiety, irritability, and agitation observed in these patients is highly relevant, as these are core symptoms of mixed episodes.12,17–19 Symptoms such as anxiety are not included in the “with mixed features” specifier of DSM-5, due to a deemed lack of specificity for mixed states alone,19 but their assessment is an important additional measure for the diagnosis and treatment of these patients. Furthermore, a recent systematic epidemiological review20 found that severe anxiety was a clinically relevant risk factor for suicide in BD, as was the mixed state (dysphoric mania with ≥3 depressive symptoms, or depressive mixed state with ≥3 hypomanic symptoms). Among psychiatric conditions, BD has the strongest association with suicide (20–30 times greater than in the general population) and may account for 25% of all completed suicides.20 Therefore, improved characterization and identification of those patients who are likely to be most at risk is a vital part of patient care.
Another informative assessment that may assist in the diagnosis of mixed episodes is the patient self-report. Indeed, it has previously been shown that patient self-assessment can accurately discriminate between the pure manic and mixed manic states in BD-I and capture some subthreshold depressive symptomatology that may not be perceived in a clinical interview.21 The current study obtained the patients’ self-rating of depressive symptoms using the validated MINI patients’ module, which presents the DSM-5 mixed features specifier in a version that can be filled in by patients.10 The patient report was in agreement with the psychiatrist’s assessment, indicating higher rates of depressive symptoms in patients with mixed features. These findings indicate that a simple patient report could play a valuable role in confirming the presence of depressive symptoms (and therefore mixed episodes) in BD-I.
An accurate diagnosis coupled with effective treatment is particularly critical for patients with mixed episodes, as they are at particular risk of severe symptoms and suicidal behavior.11 However, finding the right treatment combination to address a mix of symptoms from opposite poles can be complicated and requires considerable clinical expertise.4 The treatment of mixed states is made more difficult by the fact that the efficacy of drugs used to treat pure mania is largely unproven in the subset of patients with mixed episodes.22 Reflecting this situation, psychiatrists in the current study were more likely to be dissatisfied with the treatment response of patients with mixed features compared with that shown by patients without mixed features (ie, 0–2 depressive symptoms).
Naturalistic studies are, by definition, limited by their lack of control, but they provide important guidance concerning the “real world” situation of a disease and its treatment. The current study confirms that the presence of a mixed state of depressive symptoms during a manic episode is common in patients with BD-I. It is also associated with serious consequences in terms of severe symptoms, such as anxiety, and the incidence of suicidal behavior. The use of the new DSM-5 specifier for BD-I “with mixed features” will assist with the clinical identification of the condition and thus potentially improve the situation for patients. In addition, complementing this diagnostic approach with input from structured patient interviews is likely to be valuable in enhancing the diagnosis. The mixed state of depressive features in mania is a complex and challenging clinical picture, but improved knowledge of this patient population will help to facilitate diagnosis and drive appropriate treatment.
Acknowledgments
The study was funded by H. Lundbeck A/S, Copenhagen, Denmark. Ashfield Insight and Performance (Macclesfield, UK) provided assistance with data collection and analysis, and medical writing assistance was provided by Cambridge Medical Communication Ltd (Cambridge, UK). Financial support for these services was provided by H. Lundbeck A/S (Copenhagen, Denmark).
Disclosure
AHY has received honoraria from all major pharmaceutical companies with drugs used in affective and related disorders; he has also led investigator-initiated studies from Astra Zeneca, Eli Lilly, H. Lundbeck A/S, and Wyeth. JE is an employee of H. Lundbeck A/S.
References
Fagiolini A, Forgione R, Maccari M, et al. Prevalence, chronicity, burden and borders of bipolar disorder. J Affect Disord. 2013;148(2–3):161–169. | ||
Pini S, de Queiroz V, Pagnin D, et al. Prevalence and burden of bipolar disorders in European countries. Eur Neuropsychopharmacol. 2005;15(4):425–434. | ||
Oswald P, Souery D, Kasper S, et al. Current issues in bipolar disorder: a critical review. Eur Neuropsychopharmacol. 2007;17(11):687–695. | ||
González-Pinto A, Aldama A, Mosquera F, González Gómez C. Epidemiology, diagnosis and management of mixed mania. CNS Drugs. 2007;21(8):611–626. | ||
McElroy SL, Keck PE Jr, Pope HG Jr, Hudson JI, Faedda GL, Swann AC. Clinical and research implications of the diagnosis of dysphoric or mixed mania or hypomania. Am J Psychiatry. 1992;149(12):1633–1644. | ||
Hantouche EG, Akiskal HS, Azorin JM, Châtenet-Duchêne L, Lancrenon S. Clinical and psychometric characterization of depression in mixed mania: a report from the French national cohort of 1,090 manic patients. J Affect Disord. 2006;96(3):225–232. | ||
Akiskal HS, Bourgeois ML, Angst J, Post R, Möller H, Hirschfeld R. Re-evaluating the prevalence of and diagnostic composition within the broad clinical spectrum of bipolar disorders. J Affect Disord. 2000;59(suppl 1):S5–S30. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013. [DSM-5]. | ||
Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the clinical global impressions (CGI) scale for use in bipolar illness (BP): the CGI-BP. Psychiatry Res. 1997;73(3):159–171. | ||
Hergueta T, Weiller E. Evaluating depressive symptoms in hypomanic and manic episodes using a structured diagnostic tool: validation of a new mini international neuropsychiatric interview (M.I.N.I.) module for the DSM-5 ‘with mixed features’ specifier. Int J Bipolar Disord. 2013;1:21. | ||
Azorin JM, Aubrun E, Bertsch J, Reed C, Gerard S, Lukasiewicz M. Mixed states vs pure mania in the French sample of the EMBLEM study: results at baseline and 24 months – European mania in bipolar longitudinal evaluation of medication. BMC Psychiatry. 2009;9:33. | ||
Swann AC. Diagnosis and treatment of mixed states. In: Akiskal HS, Tohen M, editors. Bipolar Psychopharmacology: Caring for the Patient. 2nd ed. Chichester, UK: John Wiley & Sons; 2011:391–410. | ||
Goldberg JF, McElroy SL. Bipolar mixed episodes: characteristics and comorbidities. J Clin Psychiatry. 2007;68(10):e25. | ||
González-Pinto A, Barbeito S, Alonso M, et al. Poor long-term prognosis in mixed bipolar patients: 10-year outcomes in the Vitoria prospective naturalistic study in Spain. J Clin Psychiatry. 2011;72(5):671–676. | ||
Valentí M, Pacchiarotti I, Rosa AR, et al. Bipolar mixed episodes and antidepressants: a cohort study of bipolar I disorder patients. Bipolar Disord. 2011;13(2):145–154. | ||
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Text Revision (DSM-IV-TR)]. | ||
Swann AC, Secunda SK, Katz MM, et al. Specificity of mixed affective states: clinical comparison of dysphoric mania and agitated depression. J Affect Disord. 1993;28(2):81–89. | ||
Akiskal HS, Hantouche EG, Bourgeois ML, et al. Gender, temperament, and the clinical picture in dysphoric mixed mania: findings from a French national study (EPIMAN). J Affect Disord. 1998;50(2–3):175–186. | ||
Cassidy F. Anxiety as a symptom of mixed mania: implications for DSM-5. Bipolar Disord. 2010;12(4):437–439. | ||
Pompili M, Gonda X, Serafini G, et al. Epidemiology of suicide in bipolar disorders: a systematic review of the literature. Bipolar Disord. 2013;15(5):457–490. | ||
Hantouche EG, Allilaire JP, Bourgeois ML, et al. The feasibility of self-assessment of dysphoric mania in the French national EPIMAN study. J Affect Disord. 2001;67(1–3):97–103. | ||
Stahl S, Lombardo I, Loebel A, Mandel FS. Efficacy of ziprasidone in dysphoric mania: pooled analysis of two double-blind studies. J Affect Disord. 2010;122(1–2):39–45. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.