Back to Journals » Patient Preference and Adherence » Volume 9
Effect of pharmaceutical care on medication adherence of patients newly prescribed insulin therapy: a randomized controlled study
Authors Xin C, Xia Z, Jiang C, Lin M, Li G
Received 11 March 2015
Accepted for publication 26 April 2015
Published 18 June 2015 Volume 2015:9 Pages 797—802
DOI https://doi.org/10.2147/PPA.S84411
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Naifeng Liu
Chuanwei Xin, Zhongni Xia, Cheng Jiang, Mengmeng Lin, Gonghua Li
Department of Pharmacy, Tongde Hospital of Zhejiang Province, Zhejiang Academy of Traditional Chinese Medicine, Hangzhou, People’s Republic of China
Background: Poor adherence to insulin medications leads to a high rate of hospital admissions and poor health-related quality of life in the patients with diabetes mellitus. However, few strategies are effective and acceptable in improving medication adherence. The objectives of this study are to evaluate the effectiveness of pharmaceutical care by clinical pharmacists on medication adherence of patients newly prescribed insulin therapy.
Patients and methods: A single-center, prospective randomized controlled study (pharmaceutical care group and control group) was performed from January 1, 2014 to December 30, 2014. Medication adherence was measured at the baseline and up to 12 months with Morisky–Green test and computerized dispensed medication history. The absolute change in A1c vs baseline, the change of hospitalization between two groups, and the number of patients to achieve Chinese Diabetes Society (CDS) goals at the baseline were the main outcome measures.
Results: A total of 322 patients were included in the study. After the 12-month interventions, significant improvements in the medication adherence were verified for the pharmaceutical care group according to the Morisky–Green test (50.8% of adherent patients at baseline vs 80.7% of adherent patients after 12-month interventions; P<0.01) and the computerized dispensed medication history (55.2% at baseline vs 83.3% after interventions; P<0.01), while no significant changes were verified in the control group. After follow-up, the pharmaceutical care group showed a greater percent change in A1c (2.2±0.4 vs 0.8±0.2, P<0.05).
Conclusion: This study provides new evidence from a randomized controlled trial on the beneficial effect of pharmaceutical care to enhance adherence in patients newly prescribed insulin therapy. Intervention by the pharmacist might potentially improve clinical outcomes on reducing hemoglobin A1c and enhancing the number of patients fulfilling the Chinese Diabetes Society goal on hemoglobin A1c.
Keywords: medication adherence, pharmaceutical care, clinical pharmacists, insulin
Introduction
The prevalence of diabetes has increased significantly in recent decades and is now reaching epidemic proportions in the People’s Republic of China; the most recent national survey in 2010 reported that the prevalence of diabetes was 11.6%, representing an estimated 113.9 million adults in the People’s Republic of China with diabetes.1,2 Strict glycemia, good blood pressure control, and lipid management seem to be of utmost importance in order to prevent vascular complications, macrovascular and microvascular diseases. Insulin for patients with diabetes mellitus plays an important role in diabetes care and is associated with high-level self-care behavior and self-management. Also, clinical outcomes support benefits associated with early initiation and intensification of insulin therapy in patients with type 2 diabetes.3 However, poor adherence to insulin medications is common, which causes severe health complications and increased mortality.4 This is reflected, for instance, by an increase in the risk of cardiovascular diseases, neuropathy, retinopathy, nephropathy, and hospitalization rates.5
The management of diabetes is a complex, lifelong process requiring a great deal of effort on the part of the patient. Barriers for patients newly prescribed insulin therapy are numerous: the major barriers include complex treatment regimens often along with long-term therapy, adverse drug reactions, incomprehensible or confusing information, or instructions provided by the doctor; further barriers may consist of socioeconomic issues, memory impairment, psychological well-being, and personal beliefs.6,7 In spite of the crucial role of adherence to insulin for achieving therapeutic goals, a few studies have evaluated adherence of patients newly prescribed insulin.
In the United States,8 pharmacists are now adopting a crucial role in the management of diabetes mellitus. Clinical pharmacists are well positioned to help patients overcome barriers to adherence. Several studies have demonstrated that pharmaceutical care can improve adherence, self-care, and in some cases, yield a net economic return.9,10 For example, a previous systematic review examined the effects of pharmacist interventions that improve adherence to oral antidiabetic medications for type 2 diabetes mellitus, showing a positive effect on adherence.11 But in the People’s Republic of China, it was not until 2007 that the clinical pharmacy began to get long-term development. Therefore, the present study was designed to evaluate the effectiveness of pharmaceutical care among patients newly prescribed insulin therapy in the People’s Republic of China.
Methods
We conducted a single-center, prospective randomized controlled study to evaluate the pharmaceutical care on medication adherence of patients newly prescribed insulin therapy. Participants were enrolled from January 1, 2014 to December 30, 2014 in Tongde Hospital of Zhejiang Province located in Hangzhou, People’s Republic of China.
Ethical consideration
The Research Review Committee approval was obtained from Tongde Hospital of Zhejiang Province before we begin to design the study.
Patient selection
Patients were included if they were at least 18 years of age, with a diagnosis of type 2 diabetes; the patient had no evidence of a filled prescription in the insulin therapeutic during the previous 18 months; regular visits to our hospital for treatment with insulin, with up-to-date results of their routine physical and laboratory tests; and no uncontrolled psychiatric disease, severe infections, liver failure, or kidney disease.
The patients enrolled in the control group received the usual care offered in the diabetes clinic, consisting of appointments with physicians once every month. They received their prescription services without any pharmaceutical care approach.
The patients randomized into the pharmaceutical care group, besides the usual care offered, also received pharmaceutical care intervention. The intervention was composed of provision of individualized education, educative group activities, and telephone counseling. The pharmaceutical care program was developed individually, respecting the patients’ individual needs and knowledge. During the interview, the clinical pharmacist used an illustration to explain the effective use of injection devices, had a discussion with the patient about the role of medication, explained the medical testing, and reminded them of the next clinical appointment. After each interview, medication management records for the patients were established, which evaluated each participant’s preferences. Educative group activities were carried out once a month with groups of 20 patients under the supervision of the clinical pharmacist. The activities discussed some themes such as adherence, dangers of self-medication, and correct storage of insulin. During telephone counseling, the pharmacist asked about the patient’s treatment effects, explained the nature of any side effects and clarified any misconceptions. The pharmaceutical care program continued for 12 months.
Outcome measures
The medication adherence of the patients was assessed by two pharmacists (Xia and Li) at the baseline and after 12 months of follow-up, using two different methods: the Morisky–Green test translated into Chinese12 and the computerized prescribed medication history. The two pharmacists were blinded to the group allocation of the patients.
The Morisky–Green test is a validated self-reporting tool for adherence assessment, which consists of four direct questions: 1) Have you ever forgotten to inject your insulin? 2) Are you careless at times about your insulin? 3) When you feel better, do you sometimes stop injecting your insulin? 4) Sometimes if you feel worse when you inject insulin, do you stop injecting it? The patients were considered adherent to the insulin therapy when they answered “yes” to all the four questions, if the patients gave the right answer to three or less questions, they were considered nonadherent.13
The computerized prescribed insulin history during the study period was calculated. The patients with a quantity of dispensed medications within 80%–115% of the prescribed medications are considered adherent, and the patients with other values are considered nonadherent.14
Statistical analysis
The data were analyzed using statistical analysis software (SPSS© Version 19.0). Data are presented as mean ± SD or as percentages within groups. The Student’s sample t-test and chi-square test were used to compare the groups; the P-value for statistical significance was set at <0.05.
Results
Among the 240 patients recruited, a total of 227 individuals completed this study, as detailed in Figure 1. There were no statistically significant differences between the two groups in mean age, age bands, sex distribution, sociodemographic, and functional variables (Table 1).
  | Figure 1 Flow of participants through the study. |
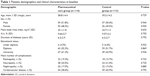  | Table 1 Patients demographics and clinical characteristics at baseline |
A high rate of nonadherent patients was observed in both the groups at the baseline. After 12 months of follow-up, the pharmaceutical care group showed a significant increase in the medication adherence according to the Morisky–Green test (50.8% of adherent patients at baseline vs 80.7% of adherent patients after 12-month interventions; P<0.01) and the computerized dispensed medication history (55.2% at baseline vs 83.3% after interventions; P<0.01), while the control group showed no significant changes (52.2% of adherent patients at baseline vs 58.4% of adherent patients after interventions; P>0.05, Morisky–Green test). No significant difference was verified between the results of the two adherence assessment tools used, as shown in Table 2.
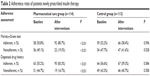  | Table 2 Adherence rates of patients newly prescribed insulin therapy |
The demographic and clinical parameters of the patients at baseline did not significantly differ as a function of the availability of hemoglobin A1c (HbA1c) values. HbA1c of the patients in the pharmaceutical care group decreased significantly by 2.2±0.4 during the 12-month study period (P<0.05), while HbA1c of the control group patients was also reduced (0.8±0.2), but not significantly, as shown in Table 3. And the pharmaceutical care group contained more patients fulfilling the Chinese Diabetes Society (CDS) goal (HbA1c <7%) than the control group (85.9% vs 55.7%; P<0.05). At 12-month follow-up, 44 patients in the control group with poorly controlled blood sugar levels resulted in hospital admission, while 22 in the pharmaceutical care group, yielding a 51.1% reduction in hospital admissions (P<0.05). Significantly more patients in the control group had one hospital admission and two hospital admissions during the study period.
  | Table 3 Hospital admissions and HbA1c, hypoglycemia, for patients during study period |
Discussion
This study assessed the effect of pharmaceutical care on medication adherence of patients newly prescribed insulin therapy and its association with clinical outcomes. The results indicate that individualized pharmaceutical care improved the medication adherence over a 12-month period, with a potential improvement in the clinical outcomes. By taking pharmaceutical care focused on the patient and working together with doctors in the process of care, the clinical pharmacists were able to provide better support for the patients newly prescribed insulin therapy.
The patients’ motivation and expectation about the likelihood of success of medical interventions are important factors to medication adherence.15 In our pharmaceutical care, multicomponent interventions, including external cognitive supports involving education strategies and behavioral component focused on the mechanism of different insulin, were tailored to the individual needs of every patient. The pharmaceutical care program encouraged the patients to develop a list of long-term and short-term goals of the insulin therapy, provided written medication instructions, promoted convenience through some reminder packaging, and conducted regular follow-up attendances to assess adherence and to motivate the patient.
The improvements in the medication adherence promoted by pharmaceutical care were associated with better clinical outcomes for the patients newly prescribed insulin therapy. The number of patients enrolled in the pharmaceutical care group fulfilling the CDS goal increased significantly after a 12-month intervention. This may be attributed to the clinical pharmacist adopting a pharmaceutical care strategy, which involved preventing and resolving drug-related problems, such as hypoglycemia.
We found that patients with higher household income, but not with more education, were less likely to skip insulin injections. This may reflect easier access to medications and supplies among the individuals with higher income, but it is also likely that higher economic status is associated with more access to higher health literacy, greater control over one’s daily routines, and better problem-solving skills. We also found that older respondents were less likely to skip insulin injections; this suggests that there are parallel aging-out processes among individuals with type 1 and type 2 diabetes.
This study is similar to other studies demonstrating the impact of pharmacist interventions to improve medication adherence. Donnelly et al reported poor adherence in 1,099 patients with type 2 diabetes; after 7 years, pharmacy record data revealed a 70.6%±17.7% mean adherence to insulin among these patients.16 Adepu and Ari showed that education provided regularly (at baseline and every 30 days for a duration of 3 months) compared to just one education session (at month 3) tended to improve adherence.17 However, the adherence between intervention and control group differed considerably at baseline. It was not reported whether the differences at baseline were adjusted in their analysis. Although prior studies have shown the value of including clinical pharmacists in general medicine teams, this study suggests that the mere presence of a clinical pharmacist is not enough to improve medication adherence. Instead, policies and procedures must be in place in order for clinical pharmacists to effectively perform job duties.
Limitations
While the present study has a number of methodological strengths, it has several limitations; this study utilized data from a single center, relatively lesser numbers of samples, and short-term period, and therefore, our patients may not have been fully representative of the overall general population of diabetic patients. Furthermore, the absence of a gold standard method to measure adherence complicated assessment of the interventions provided; some methods are useful in daily practice (easy, fast, and cheap to apply), but may overestimate adherence.18,19 In this study, the authors used two indirect methods to reduce this bias. In addition, this study was conducted in a teaching hospital in the People’s Republic of China, where participants have easy access to health care facilities; therefore, this study findings may not be applicable to other settings where health care services are more limited.
Conclusion
This study provides new evidence, from a prospective randomized controlled study, on the beneficial effect of pharmaceutical care to enhance medication adherence on the patients newly prescribed insulin therapy. The pharmacist interventions might potentially improve clinical outcomes on reducing HbA1c and enhancing the number of patients fulfilling the CDS goal on HbA1c. To confirm the generalizability of our findings, a multicenter, prospective randomized controlled study is warranted in large samples of patients newly prescribed insulin therapy.
Acknowledgments
We would like to acknowledge Dr Yunlong Tian (research question development, study selection, interpretation of results) and Mrs Ting-xia (data analysis, interpretation of results) for their involvement. This study was supported by Zhejiang Provincial Natural Science Foundation (LY14H280003).
Disclosure
The authors report no conflicts of interest in this work.
References
Hypoglycaemia Study Group UK. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50(6):1140–1147. | ||
Yang W, Lu J, Weng J, et al; China National Diabetes and Metabolic Disorders Study Group. Prevalence of diabetes among men and women in China. N Engl J Med. 2010;362(12):1090–1101. | ||
Asche CV, Bode B, Busk AK, Nair SR. The economic and clinical benefits of adequate insulin initiation and intensification in people with type 2 diabetes mellitus. Diabetes Obes Metab. 2012;14(1):47–57. | ||
Lee WC, Balu S, Cobden D, Joshi AV, Pashos CL. Medication adherence and the associated health-economic impact among patients with type 2 diabetes mellitus converting to insulin pen therapy: an analysis of third-party managed care claims data. Clin Ther. 2006;28(10):1712–1725. | ||
Patel A, MacMahon S, Chalmers J, et al; ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–2572. | ||
Rubin RR, Peyrot M, Kruger DF, Travis LB. Barriers to insulin injection therapy: patient and health care provider perspectives. Diabetes Educ. 2009;35(6):1014–1022. | ||
Farsaei S, Radfar M, Heydari Z, Abbasi F, Qorbani M. Insulin adherence in patients with diabetes: risk factors for injection omission. Prim Care Diabetes. 2014;8(4):338–345. | ||
Nkansah NT, Brewer JM, Connors R, Shermock KM. Clinical outcomes of patients with diabetes mellitus receiving medication management by pharmacists in an urban private physician practice. Am J Health Syst Pharm. 2008;65(2):145–149. | ||
Heisler M, Hofer TP, Schmittdiel JA, et al. Improving blood pressure control through a clinical pharmacist outreach program in patients with diabetes mellitus in 2 high-performing health systems: the adherence and intensification of medications cluster randomized, controlled pragmatic trial. Circulation. 2012;125(23):2863–2872. | ||
Planas LG, Crosby KM, Mitchell KD, Farmer KC. Evaluation of a hypertension medication therapy management program in patients with diabetes. J Am Pharm Assoc (2003). 2009;49(2):164–170. | ||
Antoine SL, Pieper D, Mathes T, Eikermann M. Improving the adherence of type 2 diabetes mellitus patients with pharmacy care: a systematic review of randomized controlled trials. BMC Endocr Disord. 2014;14:53. | ||
Ben AJ, Neumann CR, Mengue SS. The brief medication questionnaire and Morisky-Green test to evaluate medication adherence. Rev Saude Publica. 2012;46(2):279–289. | ||
Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. | ||
Krass I, Taylor SJ, Smith C, Armour CL. Impact on medication use and adherence of Australian pharmacists’ diabetes care services. J Am Pharm Assoc (2003). 2005;45(1):33–40. | ||
Mukama LJ, Moran A, Nyindo M, Philemon R, Msuya L. Improved glycemic control and acute complications among children with type 1 diabetes mellitus in Moshi, Tanzania. Pediatr Diabetes. 2013;14(3):211–216. | ||
Donnelly LA, Morris AD, Evans JM; DARTS/MEMO Collaboration. Adherence to insulin and its association with glycaemic control in patients with type 2 diabetes. QJM. 2007;100(6):345–350. | ||
Adepu R, Ari SM. Influence of structured patient education on therapeutic outcomes in diabetes and hypertensive patients. Asian J Pharm Clin Res. 2010;3(3):174–178. | ||
Prado JC Jr, Kupek E, Mion D Jr. Validity of four indirect methods to measure adherence in primary care hypertensives. J Hum Hypertens. 2007;21(7):579–584. | ||
Hansen RA, Kim MM, Song L, Tu W, Wu J, Murray MD. Comparison of methods to assess medication adherence and classify nonadherence. Ann Pharmacother. 2009;43(3):413–422. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
