Back to Journals » Clinical Ophthalmology » Volume 9
Effect of alcaftadine 0.25% on ocular itch associated with seasonal or perennial allergic conjunctivitis: a pooled analysis of two multicenter randomized clinical trials
Authors Ciolino JB, McLaurin E , Marsico N, Ackerman S, Williams J, Villanueva L, Hollander D
Received 7 January 2015
Accepted for publication 10 March 2015
Published 2 May 2015 Volume 2015:9 Pages 765—772
DOI https://doi.org/10.2147/OPTH.S80503
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Joseph B Ciolino,1 Eugene B McLaurin,2 Nicholas P Marsico,3 Stacey L Ackerman,4 Julia M Williams,5 Linda Villanueva,5 David A Hollander5
1Department of Ophthalmology, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston, MA, USA; 2Total Eye Care, P.A., Memphis, TN, USA; 3East West Eye Institute, Los Angeles, CA, USA; 4Philadelphia Eye Associates, Philadelphia, PA, USA; 5Allergan, Inc., Irvine, CA, USA
Purpose: Seasonal and perennial allergic conjunctivitis represent the majority of cases of ocular allergy. This analysis was designed to evaluate the efficacy and safety of once-daily alcaftadine 0.25% in preventing ocular itching associated with seasonal or perennial allergic conjunctivitis.
Subjects and methods: Pooled data from two double-masked, multicenter, placebo-controlled studies using the conjunctival allergen challenge (CAC) model of allergic conjunctivitis were analyzed. Subjects randomized to receive treatment with alcaftadine 0.25% or placebo were challenged with seasonal (grass, ragweed, trees) or perennial (cat dander, cat hair, dog dander, dust mites, cockroach) allergens, 16 hours after treatment instillation. The primary efficacy measure was subject-evaluated mean ocular itching at 3 minutes post-CAC. Secondary measures included ocular itching at 5 and 7 minutes post-CAC. The proportion of subjects with minimal itch (itch score <1) and zero itch (itch score =0), and safety were also assessed.
Results: A total of 189 subjects enrolled in the two studies were treated with alcaftadine or placebo. Overall, 129 subjects were challenged with seasonal allergens and 60 subjects were challenged with perennial allergens. Alcaftadine 0.25% achieved a statistically significant reduction in mean itch score at 3, 5, and 7 minutes post-CAC compared with placebo in subjects challenged with seasonal allergens (P<0.0001 at all time points) and those challenged with perennial allergens (P<0.0001 at all time points). A higher percentage of subjects treated with alcaftadine compared with placebo achieved minimal itch (P≤0.001 versus placebo at all time points) and zero itch (P<0.05 at all time points except 7 minutes for perennial) when challenged with either seasonal or perennial allergens. No treatment-related or serious adverse events were reported.
Conclusion: Once-daily alcaftadine 0.25% ophthalmic solution was well tolerated and demonstrated effective relief of ocular itching in subjects challenged with allergens classic for triggering either seasonal or perennial allergic conjunctivitis.
Keywords: lastacaft, seasonal allergen, perennial allergen, allergic rhinoconjunctivitis, conjunctival allergen challenge
Introduction
Allergic conjunctivitis is a common ocular condition estimated to affect 15%–40% of the general population in developed nations.1–4 Ocular allergy is characterized by an inflammatory response primarily of the conjunctival mucosa that also may affect the cornea and eyelids. Allergic conjunctivitis encompasses a group of disorders that include seasonal allergic conjunctivitis (SAC), perennial allergic conjunctivitis (PAC), as well as more severe and chronic conditions of vernal keratoconjunctivitis and atopic keratoconjunctivitis.5,6 Acute allergic conjunctivitis is primarily caused by IgE-mediated mast cell degranulation and the subsequent release of histamine and other inflammatory mediators. Release of histamine induces ocular itching (the hallmark symptom of ocular allergy), as well as other ocular signs and symptoms, including redness, eyelid swelling, chemosis, and tearing. These ocular symptoms are commonly accompanied by nasal symptoms or rhinitis, and often collectively referred to as allergic rhinoconjunctivitis.7–9 Ocular itching is directly related to the action of histamine on H1 receptors in the conjunctiva.10 Other allergic symptoms have been attributed to the action of H1 or H2 receptors on the vasculature.11,12
SAC and PAC account for the majority of cases of ocular allergy.1,6,13 Both conditions result from IgE cross-linking on the surface of mast cells following ocular exposure to allergen and present with similar signs and symptoms. SAC and PAC may differ in the specific allergen(s) that cause the reaction in an individual and in the duration of symptoms. SAC, typically characterized by an acute to subacute onset triggered primarily by tree, grass, and weed pollen, is more common and occurs during periods of high pollen counts. In contrast, PAC tends to occur throughout the year, caused typically by indoor antigens such as dust, molds, or animal dander.4,6,13,14 Ocular symptoms experienced by individuals suffering from allergic conditions can significantly impact daily activities and quality of life.15–17
Alcaftadine 0.25% ophthalmic solution (Lastacaft®; Allergan, Inc., Irvine, CA, USA) is a once-daily, dual-action antiallergic that inhibits histamine receptor activation and stabilizes mast cells and has been approved for the prevention of itching associated with allergic conjunctivitis in the United States.18 In preclinical investigations, alcaftadine exhibited high affinity for both H1 and H2 receptors, as well as in vitro antagonism of H4 receptors.19 Alcaftadine 0.25% has been shown to be safe and effective in the prevention of ocular itching using the conjunctival allergen challenge (CAC) model of allergic conjunctivitis. In pivotal studies, when compared with placebo, alcaftadine 0.25% was superior at reducing ocular itching at 15 minutes and 16 hours after instillation.20,21
Two similarly designed studies were conducted comparing the efficacy and duration of action of once-daily alcaftadine 0.25% and olopatadine 0.2%, and placebo using the CAC model.22–24 Subjects in the two studies were required to have a history of ocular allergies and at least one positive skin test to one or more of the following either seasonal or perennial allergens: cat hair, cat dander, dog dander, cockroach, dust mites, grasses, ragweed, and trees. Subjects may have been challenged with any of these allergens during the course of the two studies. Pooled analysis of data from the two studies demonstrated that alcaftadine 0.25% achieved lower overall ocular mean itching scores compared with placebo and olopatadine 0.1%, 16 hours after treatment instillation using the CAC model.25 The objective of the current analysis of pooled data from these two similarly designed studies was to evaluate the efficacy of alcaftadine 0.25% compared with placebo in the subgroups of subjects challenged with allergens characteristic of SAC or PAC.
Materials and methods
Study design
Data collected from two multicenter, double-masked, randomized, placebo-controlled trials, conducted between October 2011 and December 2012 (Clinicaltrials.gov identifier: NCT01470118 and NCT01732757), in five centers across the United States were pooled for analysis.22–24 Both studies were reviewed and approved by an independent review board (Alpha IRB; San Clemente, CA, USA) and conducted in accordance with the Declaration of Helsinki and International Conference of Harmonisation Guidelines for Good Clinical Practice. All subjects enrolled in the study provided written informed consent and signed authorization for the Health Insurance Portability and Accountability Act prior to initiation of any procedures or treatment.
Subject eligibility criteria
Subjects were enrolled in the two clinical studies if they were at least 10 years of age, had a history of ocular allergies, and reacted positively in a skin test in the past 24 months to cat hair, cat dander, grasses, ragweed, dog dander, cockroach, dust mite, or trees. Eligible subjects had a best-corrected visual acuity of 0.6 or better on the logMAR scale in each eye, measured using the Early Treatment Diabetic Retinopathy Study chart, and displayed a positive bilateral CAC reaction (scores ≥2 for itching and redness in the conjunctival vessel bed) within the first 10 minutes of the last instillation of allergen on visit 1 and in at least two of the three time points at visit 2 as described.
Key exclusion criteria included subjects displaying symptoms of clinically active allergic conjunctivitis at the start of each visit, defined as itching or a redness score >1 in any vessel bed, and subjects with a clinically significant ocular or systemic condition, or infection, which may confound study data. Individuals who had ocular surgery within the last 3 months or refractive surgery within the last 6 months or had any known allergy, contraindications, or sensitivity to the study medications were also excluded from the studies.
Study treatment and clinical assessments
Subject assessments were conducted at three study visits that were identical in the two trials. These assessments were included in the pooled analysis. At the first visit (day −21±3) or titration visit, subjects were challenged with increasing concentration of allergens followed by the subject rating ocular itching severity after 10 minutes. Subjects were challenged with seasonal or perennial allergens to which they had known sensitivity; allergens used for conjunctival challenge in both studies included cat dander, dog dander, cockroach, dust mite, grass, ragweed, and trees. Cat hair was also included as a possible allergen in one of the two studies. A CAC reaction was considered positive when the score for both ocular itching and conjunctival vessel bed redness was ≥2.0. Itching was graded by the subject on a 0–4 scale, which allowed half increments for measurements, and conjunctival redness was scored by the investigator on a 0–4 scale for ocular redness.
At the second visit (day −14±3) or confirmation visit, subjects still satisfying eligibility criteria were challenged with the final concentration of allergen from the first visit to obtain baseline data. Following CAC with seasonal or perennial allergens, subjects rated ocular itching at 3, 5, and 7 minutes and those meeting qualifying criteria (post-challenge bilateral itching ≥2 and bilateral conjunctival redness ≥2 at two of the three time points assessed by the investigator [7 minutes, 15 minutes, and 20 minutes]) continued to the third visit.
The third visit (day 0) occurred approximately 2 weeks after visit 2, and subjects were randomized (1:1:1) to receive treatment with alcaftadine 0.25% ophthalmic solution (Lastacaft®; Allergan, Inc.), olopatadine 0.2% ophthalmic solution (Pataday®; Alcon Laboratories, Inc., Fort Worth, TX, USA), and placebo (0.3% hydroxypropyl methylcellulose [Tears Naturale® II; Alcon Laboratories, Inc.]). Each eye received a single drop of the study medication. Subjects then returned 15.5 hours later and were challenged 16+1 hours, using the allergen (seasonal or perennial) and dose established to elicit an allergic response at visits 1 and 2.
After all evaluations were completed at the end of each visit, the use of over-the-counter antiallergy eye drop Visine-A® was permitted. Systemic and/or topical nonsteroidal anti-inflammatory drugs, aspirin or aspirin-containing products, prescription, over-the-counter or homeopathic antiallergy therapies (including over-the-counter sleeping aids that contain an antihistamine and all antihistamines), all other topical ophthalmic preparations (including tear substitutes), and H1 antagonist antihistamines/mast cell stabilizers (ie, olopatadine) were not permitted up to 72 hours prior to the start of the study or during the course of the study. Systemic and/or topical corticosteroids were not permitted up to 14 days prior to the start of the study or during the course of the study.
Efficacy and safety endpoints
The primary efficacy measure was ocular itching, 16 hours after instillation of study medication, evaluated by the subject at 3 minutes post-CAC (primary endpoint) and at 5 and 7 minutes post-CAC (secondary endpoints). For safety assessment, the incidence of adverse events was monitored and the severity and relationship to the study drug was determined by the Investigator. Adverse events were coded to system organ class and preferred terms using the Medical Dictionary for Regulatory Activities, version 13.1.
Data analysis and statistical methods
All subjects who were randomized comprised the intent-to-treat population used for efficacy analyses. The safety population included all randomized subjects who received at least one dose of the study treatment. Both eyes of each subject challenged with seasonal or perennial allergens were used for statistical summaries and analyses. Categorical variables were summarized using frequencies and percentages, and continuous variables were summarized using descriptive statistics, including the number of observations, mean, standard deviation, median, minimum, and maximum values. Hypothesis testing, unless otherwise indicated, was performed at the 5% significance level of type I error for two-sided tests. The last observation carried forward method was used to handle missing and incomplete efficacy data for the primary measure.
The primary efficacy measure of ocular itching was summarized by visit, time point, and treatment group using descriptive statistics. The differences in the means between treatment groups were calculated, and mean ocular itching scores for each of the treatments were compared using two-sample t-tests. Additionally, the nonparametric Wilcoxon rank-sum test at each time point and repeated measures analysis of covariance model accounting for treatment and repeated time measurements within each visit were performed. Predefined analyses on the primary efficacy measure included comparisons of the number of subjects in each group with minimal itch (defined as itch score <1), and the number of subjects with zero itch (defined as itch score =0). Fisher’s exact test was conducted for comparisons at each time point (3, 5, and 7 minutes) for alcaftadine versus placebo. In the current analysis, grass, ragweed, and trees were categorized as seasonal allergens, and cat dander, dog dander, cat hair, dust mites, and cockroach were categorized as perennial allergens. Safety findings were tabulated and summarized using descriptive statistics. Statistical analyses were performed using SAS® software, version 9.2 (SAS Institute Inc., Cary, NC, USA).
Results
Subject disposition and baseline characteristics
A total of 284 subjects were randomized in the two pooled studies and 189 were treated with either alcaftadine 0.25% ophthalmic solution or placebo (Figure 1). Of the 96 subjects who were treated with alcaftadine 0.25%, 63 were challenged with seasonal allergens and 33 with perennial allergens. Of the 93 subjects who received placebo, 66 were challenged with seasonal allergens and 27 with perennial allergens. Overall completion rate was high among the two treatment groups (93.8% alcaftadine 0.25% and 97.8% placebo), and only three subjects withdrew from the study due to adverse events (two in the alcaftadine 0.25% group and one in the placebo group). Baseline characteristics were similar between the alcaftadine 0.25% and placebo treatments groups with respect to age, sex, ethnicity, and race, although some differences were observed in iris color (Table 1).
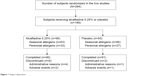  | Figure 1 Subject disposition. |
Efficacy of alcaftadine on ocular itching induced by seasonal or perennial allergens
Treatment with alcaftadine 0.25%, 16 hours prior to allergen challenge, significantly reduced mean ocular itching compared with placebo at 3, 5, and 7 minutes post-CAC in subjects challenged with seasonal or perennial allergens (Figure 2). Differences in mean ocular itching scores between alcaftadine 0.25% and placebo were statistically significant at 3, 5, and 7 minutes post-CAC (P<0.0001 for all time points) for both seasonal and perennial allergens subgroups (Table 2). Alcaftadine 0.25%-treated subjects consistently demonstrated greater percentage reduction in itching from baseline at 3, 5, and 7 minutes post-CAC (seasonal allergens: −79.1%, −73.0%, and −70.4%, respectively; perennial allergens: −85.0%, −76.6%, and −71.0%, respectively) compared with placebo-treated subjects (seasonal allergens: −26.0%, −24.8%, and −32.0%, respectively; perennial allergens: −18.2%, −22.4%, and −26.0%, respectively), with similar efficacy demonstrated between those subjects challenged with seasonal allergens and those subjects challenged with perennial allergens.
Ocular itching was also assessed by comparing the proportion of subjects who met the criteria of minimal itch (itch score <1) and zero itch (itch score =0) at the three time points measured post-CAC (3, 5, and 7 minutes). Significantly greater proportions of alcaftadine 0.25%-treated subjects compared with placebo-treated subjects achieved criteria for minimal itch (P≤0.001; Figure 3A) and zero itch (P<0.05; Figure 3B) in the seasonal allergens subgroup. Similarly, among subjects who were challenged with perennial allergens, significantly higher proportions of alcaftadine 0.25%-treated subjects compared with placebo-treated subjects achieved an itch score <1 (P≤0.001; Figure 3C) and itch score =0 (P<0.05 except at the 7 minutes time point; Figure 3D) compared with subjects receiving placebo.
Ocular itching was further evaluated by analyzing the distribution of raw subject-reported itch scores at baseline and 16 hours post-treatment. For this analysis, all itch score data of each eye were included for all time points (3, 5, and 7 minutes) – a leftward shift in frequency of scores indicates improvement in magnitude of relief and percentage of subjects who had their symptoms alleviated. In both seasonal and perennial allergens subgroups, a larger proportion of alcaftadine 0.25%-treated subjects reported lower itch scores compared with placebo-treated subjects 16 hours after treatment instillation, and a greater leftward shift was observed following treatment with alcaftadine than placebo (Figure 4).
Safety outcomes
In the pooled population, a total of 11 adverse events were reported among the 189 subjects receiving alcaftadine 0.25% and placebo. Four alcaftadine 0.25%-treated subjects and one placebo-treated subject experienced at least one adverse event during the course of the studies. There were no treatment-related adverse events recorded and no serious adverse events occurred in the two pooled studies.
Discussion
Both SAC and PAC can cause significant discomfort, reduce quality of life, and lead to a loss of productivity, particularly during the spring and fall allergy seasons.15–17 Effectively treating the signs and symptoms of allergic conjunctivitis26 and limiting the onset of future symptoms via minimizing exposure to specific allergens27 have been shown to improve quality of life in patients with ocular allergy. The ocular manifestations of both SAC and PAC are secondary to mast cell degranulation and subsequent allergic inflammation in sensitized individuals. Once sensitized, exposure to either a seasonal or perennial allergen may elicit a classic allergic conjunctivitis response within minutes. Therefore, critical to improving a patient’s quality of life is a safe and effective treatment that has a rapid onset of action and is effective against both seasonal and perennial allergens.
Topical ophthalmic antihistamines are the primary treatment option for patients with allergic conjunctivitis. With antagonistic activity against H1, H2, and H4 receptors, alcaftadine is a dual-action antiallergic agent that directly inhibits histamine receptor activation and indirectly reduces allergic responses by stabilizing mast cells.28,29 The role of H4 receptors in allergic conjunctivitis has not been fully elucidated; in vitro studies suggest that histamine binding to H4 receptors may mediate eosinophil chemotaxis.30 In vivo studies have also suggested that H4 receptors play a role in mediating inflammatory and pruritic responses.31
In the current analysis of pooled data from two, large, similarly designed clinical studies, alcaftadine 0.25% was well tolerated and demonstrated significant reduction in ocular itching induced by both seasonal and perennial allergens at all time points (3, 5, and 7 minutes) measured after conjunctival challenge with allergen using the CAC model. In addition, the reduction in itching by alcaftadine was similar between those subjects challenged with seasonal allergens and those challenged with perennial allergens. Significantly higher proportions of subjects challenged with seasonal or perennial allergens achieved minimal itch (itch score <1) or zero itch (itch score =0) after treatment with alcaftadine 0.25% compared with placebo. Alcaftadine was shown to have a rapid onset of action upon challenge with both seasonal and perennial allergens, up to 16 hours post drop instillation. This rapid and sustained effect of alcaftadine may be because of its ability to prevent loss of epithelial tight junction proteins (zonula occludens-1, E-cadherin) and to reduce eosinophil infiltration, as has been shown in animal models of allergic conjunctivitis.19
Limitations of this study are inherent in any pooled analysis, though the two studies had similar designs. In addition, there was no prespecified percentage of patients to be tested in either study with a specific type of allergen. Approximately two-thirds of patients in the alcaftadine and control groups were challenged with allergens categorized as seasonal allergens and the remaining patients were challenged with perennial allergens. While reduction of itching by alcaftadine was similar in subjects challenged with either seasonal or perennial allergens, the smaller sample size in the perennial allergen population likely accounted for the lack of statistical difference at the 7-minute time point in the percent of patients with zero itch analysis.
Overall, alcaftadine is well tolerated and is effective in reducing ocular itching associated with allergic conjunctivitis in response to both seasonal and perennial allergens.
Acknowledgments
This study was sponsored by Allergan, Inc., Irvine, CA, USA. Writing and editorial assistance was provided to the authors by Kakuri Omari, PhD, of Evidence Scientific Solutions, and funded by Allergan, Inc., Irvine, CA, USA. All authors met the ICMJE authorship criteria. Neither honoraria nor payments were made for authorship.
Disclosure
Joseph B Ciolino is supported by a Career Development Award from Research to Prevent Blindness, Inc., and the National Eye Institute. Eugene B McLaurin has received research support from Aciex, Acucela, Alcon, Allergan, Inc., AstraZeneca, Bausch & Lomb, Inotek Pharmaceuticals, InSite Vision, and Lexicon Pharmaceuticals. Stacey L Ackerman has received research support from Aciex, Alcon, Allergan, Inc., and Bausch & Lomb. Julia M Williams, Linda Villanueva, and David A Hollander are employees of Allergan, Inc., Irvine, CA, USA. Nicholas P Marsico has no conflict to disclose related to this work.
References
Butrus S, Portela R. Ocular allergy: diagnosis and treatment. Ophthalmol Clin North Am. 2005;18(4):485–492. | ||
Katelaris CH, Bielory L. Evidence-based study design in ocular allergy trials. Curr Opin Allergy Clin Immunol. 2008;8(5):484–488. | ||
Rosario N, Bielory L. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2011;11(5):471–476. | ||
Wong AH, Barg SS, Leung AK. Seasonal and perennial allergic conjunctivitis. Recent Pat Inflamm Allergy Drug Discov. 2014;8(2):139–153. | ||
Bielory L. Ocular allergy overview. Immunol Allergy Clin North Am. 2008;28(1):1–23,v. | ||
La Rosa M, Lionetti E, Reibaldi M, et al. Allergic conjunctivitis: a comprehensive review of the literature. Ital J Pediatr. 2013;39:18. | ||
Abelson MB, Smith L, Chapin M. Ocular allergic disease: mechanisms, disease sub-types, treatment. Ocul Surf. 2003;1(3):127–149. | ||
Akdis CA, Blaser K. Histamine in the immune regulation of allergic inflammation. J Allergy Clin Immunol. 2003;112(1):15–22. | ||
Leonardi A, Bogacka E, Fauquert JL, et al. Ocular allergy: recognizing and diagnosing hypersensitivity disorders of the ocular surface. Allergy. 2012;67(11):1327–1337. | ||
Udell IJ, Abelson MB. Animal and human ocular surface response to a topical nonimmune mast-cell degranulating agent (compound 48/80). Am J Ophthalmol. 1981;91(2):226–230. | ||
Abelson MB, Udell IJ. H2-receptors in the human ocular surface. Arch Ophthalmol. 1981;99(2):302–304. | ||
Smith JA, Mansfield LE, de Shazo RD, Nelson HS. An evaluation of the pharmacologic inhibition of the immediate and late cutaneous reaction to allergen. J Allergy Clin Immunol. 1980;65(2):118–121. | ||
Gomes PJ. Trends in prevalence and treatment of ocular allergy. Curr Opin Allergy Clin Immunol. 2014;14(5):451–456. | ||
Offiah I, Calder VL. Immune mechanisms in allergic eye diseases: what is new? Curr Opin Allergy Clin Immunol. 2009;9(5):477–481. | ||
Virchow JC, Kay S, Demoly P, Mullol J, Canonica W, Higgins V. Impact of ocular symptoms on quality of life (QoL), work productivity and resource utilisation in allergic rhinitis patients – an observational, cross sectional study in four countries in Europe. J Med Econ. 2011;14(3):305–314. | ||
Blaiss MS. Allergic rhinoconjunctivitis: burden of disease. Allergy Asthma Proc. 2007;28(4):393–397. | ||
Palmares J, Delgado L, Cidade M, Quadrado MJ, Filipe HP. Allergic conjunctivitis: a national cross-sectional study of clinical characteristics and quality of life. Eur J Ophthalmol. 2010;20(2):257–264. | ||
Lastacaft (alcaftadine ophthalmic solution) 0.25% [Package insert]. Irvine, CA: Allergan Inc.; 2011. | ||
Gallois-Bernos A, Thurmond RL. Pharmacology of alcaftadine, a new antihistamine for ocular allergy. Invest Ophthalmol Vis Sci. 2011; 52:e6426. | ||
Greiner JV, Edwards-Swanson K, Ingerman A. Evaluation of alcaftadine 0.25% ophthalmic solution in acute allergic conjunctivitis at 15 minutes and 16 hours after instillation versus placebo and olopatadine 0.1%. Clin Ophthalmol. 2011;5:87–93. | ||
Torkildsen G, Shedden A. The safety and efficacy of alcaftadine 0.25% ophthalmic solution for the prevention of itching associated with allergic conjunctivitis. Curr Med Res Opin. 2011;27(3):623–631. | ||
Ackerman S, D’Ambrosio F Jr, Greiner JV, Villanueva L, Ciolino JB, Hollander DA. A multicenter evaluation of the efficacy and duration of action of alcaftadine 0.25% and olopatadine 0.2% in the conjunctival allergen challenge model. J Asthma Allergy. 2013;6:43–52. | ||
McLaurin EB, Marsico NP, Ciolino JB, Williams JM, Hollander DA. Alcaftadine 0.25% versus Olopatadine 0.2% in the Prevention of Ocular Itching in Allergic Conjunctivitis. Baltimore, MD: Paper presented at: Annual Scientific Meeting; November 7–11, 2013; American College of Allergy, Asthma and Immunology; 2013. | ||
McLaurin EB, Marsico NP, Ciolino JB, Williams JM, Hollander DA. Alcaftadine 0.25% versus Olopatadine 0.2% in Prevention of Ocular Itching Due to Allergic Conjunctivitis in a CAC™ Model. New Orleans, LA: Paper presented at: Annual Meeting; November 16–19, 2013; American Academy of Ophthalmology; 2013. | ||
McLaurin EB, Marsico NP, Ackerman SL, et al. Ocular itch relief with alcaftadine 0.25% versus olopatadine 0.2% in allergic conjunctivitis: pooled analysis of two multicenter randomized clinical trials. Adv Ther. 2014;31(10):1059–1071. | ||
Scoper SV, Berdy GJ, Lichtenstein SJ, et al. Perception and quality of life associated with the use of olopatadine 0.2% (Pataday) in patients with active allergic conjunctivitis. Adv Ther. 2007;24(6):1221–1232. | ||
Stillerman A, Nachtsheim C, Li W, Albrecht M, Waldman J. Efficacy of a novel air filtration pillow for avoidance of perennial allergens in symptomatic adults. Ann Allergy Asthma Immunol. 2010;104(5):440–449. | ||
Namdar R, Valdez C. Alcaftadine: a topical antihistamine for use in allergic conjunctivitis. Drugs Today (Barc). 2011;47(12):883–890. | ||
Wade L, Bielory L, Rudner S. Ophthalmic antihistamines and H1-H4 receptors. Curr Opin Allergy Clin Immunol. 2012;12(5):510–516. | ||
Ling P, Ngo K, Nguyen S, et al. Histamine H4 receptor mediates eosinophil chemotaxis with cell shape change and adhesion molecule upregulation. Br J Pharmacol. 2004;142(1):161–171. | ||
Thurmond RL, Gelfand EW, Dunford PJ. The role of histamine H1 and H4 receptors in allergic inflammation: the search for new antihistamines. Nat Rev Drug Discov. 2008;7(1):41–53. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





