Back to Journals » Medical Devices: Evidence and Research » Volume 8
Drug-eluting stents with biodegradable polymer for the treatment of patients with diabetes mellitus: clinical outcome at 2 years in a large population of patients
Authors Wiemer M, Danzi GB, West N, Voudris V, Koning R, Hoffmann S, Lombardi M, Mauri J, Babic R, Witherow F, Mauri Ferre F
Received 8 May 2014
Accepted for publication 4 September 2014
Published 18 February 2015 Volume 2015:8 Pages 153—160
DOI https://doi.org/10.2147/MDER.S67399
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Scott Fraser
Marcus Wiemer,1 Gian Battista Danzi,2 Nick West,3 Vassilios Voudris,4 René Koning,5 Stefan Hoffmann,6 Mario Lombardi,7 Josepa Mauri,8 Rade Babic,9 Fraser Witherow10
On behalf of the NOBORI 2 Investigators
1Department of Cardiology, Heart and Diabetes Center North Rhine–Westphalia, Ruhr University Bochum, Bad Oeynhausen, Germany; 2Ospedale Maggiore Policlinico, Milan, Italy; 3Papworth Hospital, Cambridge, UK; 4Onassis Cardiac Surgery Center, Athens, Greece; 5Clinique Saint Hilaire, Rouen, France; 6Vivantes Netzwerk für Gesundheit GmbH, Berlin, Germany; 7Azienda Ospedaliera Villa Sofia, Palermo, Italy; 8Hospital Universitari Germans Trias i Pujol, Badalona, Spain; 9Institute for Cardiovascular Diseases Dedinje, Belgrade, Serbia; 10Dorset County Hospital, Dorchester, UK
Objective: This study investigates the safety and efficacy of a third-generation drug-eluting stent (DES) with biodegradable polymer in the complex patient population of diabetes mellitus (DM).
Clinical trial registration: ISRCTN81649913.
Background: Percutaneous coronary interventions in patients with DM are associated with a higher incidence of death, restenosis, and stent thrombosis as compared to non-diabetic patients. The use of a DES has been shown to improve outcomes in diabetic patients.
Methods: Out of 3,067 patients, enrolled in 126 centers worldwide in the NOBORI 2 registry, 888 patients suffered from DM, 213 of them (14%) being insulin-dependent DM (IDDM). Two years’ follow-up has been completed in this study.
Results: At 1- and 2-year follow-up, 97% and 95% of the patients, respectively, were available. The reported target lesion failure (TLF) rates at 1- and 2-year follow-up were 6.0% and 7.2% in the DM group, respectively, and 3.0% and 4.2% in the non-DM group, respectively (P<0.001 for both years). Inside the DM group, the TLF rates of 9.9% and 11.7% at the 1- and 2-year follow-ups, respectively, in patients with IDDM were significantly higher than the TLF rates of 4.7% and 5.8%, respectively, in the non-IDDM subgroup (P<0.01 for both years). The rate of stent thrombosis at the 2-year follow-up was 1.0% in the DM group and 0.7% in non-DM patients. There were no cases of late, or very late stent thrombosis in IDDM patients.
Conclusion: The Nobori DES performed well in patients with DM. As expected, patients with DM, particularly those with IDDM, had worse outcomes. However, the absence of late, and very late stent thrombosis in IDDM patients merits further investigation, as this finding might have significant clinical value.
Keywords: diabetes mellitus, percutaneous coronary intervention, biodegradable polymer, drug-eluting stents
Introduction
Patients with diabetes mellitus (DM) subjected to percutaneous coronary intervention (PCI) are at increased risk for adverse outcomes, including restenosis repeat revascularization, myocardial infarction (MI), and mortality. They have more complex and severe lesions, more extensive and diffuse atherosclerosis, increased prevalence of multi- or triple-vessel disease, smaller caliber vessels, and a higher incidence of left main disease.1–4 The efficacy of drug-eluting stents (DES) in reducing restenosis and ischemia-driven repeat revascularization procedures has been demonstrated in this patient population, with a greater absolute reduction in repeat revascularization in patients with DM compared to those without DM.5–7 Despite the proven efficacy, there exists the safety concerns particularly related to late stent thrombosis after implantation of the first-generation DES.8 It has been suggested that their permanent polymers containing the anti-proliferative drug were partly responsible for delayed vascular healing, and were thus a possible substrate for stent thrombosis.9,10 This is of concern for patients with DM, as the disease is usually associated with a pro-thrombotic state, thus rendering them at increased risk of thrombotic events.11
The Nobori stent system incorporates a biodegradable polymer carrier containing the anti-proliferative drug Biolimus A9™ (Biosensors International, Singapore, Singapore) that is only applied on the abluminal surface of the stent platform. By reducing contact with the blood, the abluminal coating might enhance the attachment of endothelial progenitor cells from the peripheral circulation or in-growth of endothelial tissue from the distal and proximal edges of the stent.12 In patients with de novo lesions in native coronary arteries, results from numerous studies have confirmed the very good safety and efficacy profiles of the stent.12–14 However, its efficacy in patients with DM has not been fully established.
Accordingly, the aim of the present work was to evaluate the performance of the Nobori stent system in patients with DM enrolled in the NOBORI 2 registry. The influence of insulin therapy was also evaluated, as patients with insulin-dependent DM (IDDM) are known to be at higher risk of adverse events.15
Materials and methods
Patient population
The NOBORI 2 study enrollment strategy aimed to ensure a patient population representative of daily practice. All investigators were requested to enroll consecutive patients suitable for treatment with DES according to hospital standard procedures, matching available sizes of Nobori DES. The studied population consisted of 3,067 patients enrolled between April 2008 and March 2009 in 126 centers in Europe and Asia. Through data entry in the electronic case report form, based on prior diagnosis, patients were automatically assigned to predefined analysis group of diabetic patients, and if they were on insulin therapy they were allocated to IDDM subgroup. No specific laboratory confirmation was requested for confirmation of DM. The study was conducted according to the Declaration of Helsinki, ISO 14155 and respecting all country-specific regulatory requirements. The protocol was reviewed and approved by the ethics committee of each participating hospital and all patients gave written informed consent.
The Nobori Biolimus A9-eluting stent
The Nobori DES system comprises four components: 1) the bare metal stent platform; 2) the delivery catheter; 3) the biodegradable drug carrier (polylactic acid); and 4) an anti-proliferative substance, Biolimus A9™. Contrary to other DES, the drug polymer matrix is applied only abluminally (toward the vessel wall). The design of the Nobori DES stent system has been described in details previously.12–14 The Nobori stent was available in lengths from 8 to 28 mm and in diameters of 2.5, 3.0, and 3.5 mm.
Coronary stent procedure
Patients’ medication regimen, percutaneous access, lesion preparation, and stent implantations were performed according to hospital routine practice with no recommendation for any aspect of it. The treatment of multiple target vessels and staged procedures were allowed. Peri-procedural clopidogrel was given to 99.6% of the patients in addition to aspirin. Glycoprotein IIb/IIIa inhibitor was administered in 17% of all patients. A post-procedural electrocardiogram and the measurement of cardiac enzymes were recommended. All patients had an additional assessment of comorbidities using the Charlson comorbidity index, which was described before.16
Patient follow-up
All patients were followed through hospital discharge and were scheduled for follow-up evaluations (hospital visit or telephone assessment) at 1, 6, and 12 months, and annually up to 5 years post-procedure. No mandatory angiographic follow-ups were planned in this study. During the follow-up contacts, information about patients’ clinical condition, adverse events, hospitalizations, and changes to concomitant (cardiac and antiplatelet) medications were collected.
Study management
Data were collected on standardized electronic case report forms (KIKA Medical, Boston, MA, USA), monitored online (100%), and on-site (30%). An independent clinical event committee reviewed and adjudicated all major adverse cardiac events. All baseline angiograms were analyzed by an independent core laboratory (CorExpert, Belgrade, Serbia). The corresponding author had full access to all data in the study and takes final responsibility for the decision to submit for publication.
Study endpoints
The key endpoints of the study were target lesion failure (TLF), a device-oriented composite endpoint, defined as cardiac death, MI (Q-wave and non-Q-wave not clearly attributable to non-target vessels), and clinically driven target lesion revascularization (TLR); patient-oriented composite endpoint (POCE), defined as mortality of any cause, any MI and any coronary revascularization; stent thrombosis (definite and probable according to Academic Research Consortium [ARC] definitions); a composite of hard endpoints of cardiac death and MI; and target lesion and target vessel revascularization (TVR) at 12 months and yearly up to 5 years’ post-procedure.
Statistical analysis
Data were presented as percentages and 95% confidence intervals for categorical variables, and means and standard deviations for continuous variables. All analyses were performed by an independent statistical office (SBD Analytics, Bekkevoort, Belgium) using SAS software, version 9.13 (SAS Institute Inc., Cary, NC, USA). All statistical tests were two-tailed with P≤0.05 considered to be statistically significant. Differences between IDDM and non-IDDM (NIDDM) patients were analyzed using Fisher’s exact test for binary variables, and Wilcoxon rank sum test for continuous variables.
Results
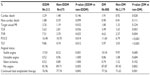
In the NOBORI 2 study, the subgroup of patients with DM consisted of 888 patients; 213 of them suffered from IDDM. The DM group contained significantly more women than the non-DM group (27.7% versus [vs] 19.7%, P<0.0001). The occurrence of hypercholesterolemia, hypertension, congestive heart failure, and peripheral vascular disease was also significantly higher in the DM group (Table 1). At baseline, DM patients presented more often with silent ischemia as compared to non-DM patients (17.38% vs 14.13%, P=0.026).
As expected, patients with DM had a significantly higher Charlson comorbidity index.
Baseline procedural details, quantitative coronary angiography results, and lesion characteristics
The mean number of diseased vessels per DM patient was 1.83±0.78 vessels. The number of lesions detected and treated per patient was 2.18±1.17 and 1.44±0.69, respectively. All these numbers were significantly higher in the DM group as compared to the non-DM group; however, the difference between diseased and treated vessels was higher in DM group. The mean lesion length was shorter in the DM group, mainly due to shorter lesions in NIDDM patients (Table 2). The reference vessel diameter of treated arteries and minimum luminal diameter post-procedure were significantly smaller in patients with DM, with no difference between the IDDM and NIDDM subgroups (Table 2).
In the DM subgroup, significantly more calcified (30.24% vs 24.27%, P<0.001) and tortuous (10.31% vs 6.67%, P<0.001) lesions were treated as compared to the non-DM group (data not shown). Pre-dilatation of the lesion was also more often performed in the DM group (73.5% vs 70.5%, P=0.043). This was mainly due to a higher percentage of pre-dilatation in the IDDM subgroup (79.06% vs 71.76%, P=0.011).
Clinical outcomes at 1-year follow-up
At 1-year follow-up, 97% of the patients were available. The TLF rate in the DM group was 6.0%, and the main contributing factors were cardiac death and TLR. The value was significantly higher than the one observed in the non-DM group (3.0%). This was mainly driven by events in the IDDM subgroup of DM patients (Table 3). In the DM group, 17 people died of a cardiac cause (seven IDDM patients and ten NIDDM patients), and 16 patients suffered from a target vessel-related MI.
In the DM group, thrombosis in the study stent (definite and probable according to the ARC definitions) occurred in seven patients (two patients with IDDM and five patients with NIDDM). All stent thromboses happened within 30 days of the baseline procedure (early). These values were not significantly different from the ones reported for the non-DM group. At 1-year follow-up, 87.9% of the DM patients and 87.4% of non-DM patients were free from angina. However, within the DM group, significantly less IDDM patients were angina free. This was mainly due to a high occurrence of stable angina in this subset of patients (17.0% vs 8.5%, P=0.001) (Table 3).
Clinical outcomes at 2-year follow-up
At 2-years follow-up, 95% of the patients were available. The TLF rate in the DM group was 7.2%, while it was 4.2% in the non-DM group (P<0.001). As observed at 1-year follow-up, the main contributing factors for both parameters were cardiac death and TLR.
The rate of POCE was also significantly higher in DM patients (Figure 1, Table 4). These higher rates in the DM group were again mainly driven by more events in the IDDM subgroup. After the 1-year follow-up, six additional DM patients died because of a cardiac cause (two IDDM patients and four NIDDM patients), and three patients died due to a non-cardiac cause. The number of patients who suffered from a target vessel-related MI did not change in the DM group, while it increased by two patients in the non-DM group.
Very late study stent thrombosis occurred in two patients in the NIDDM subgroup and none in the IDDM patients (Tables 3 and Figure 2). At 2-year follow-up, 87.3% of the DM patients were free from angina and, as at 1-year follow-up, significantly less IDDM patients were angina free, mainly due to a high occurrence of stable angina in this subset of patients (15.9% vs 9.0%, P=0.013). Significantly more DM patients were still on dual antiplatelet therapy as compared to non-DM patients (39.1% vs 31.1%, P<0.001) (Table 4).
Patients with chronic heart failure (CHF) (54 patients) had higher adverse outcomes: at 2-year follow-up, TLF was 14.8% in CHF patients and 8.0% in non-CHF patients; however, the difference was not statistically significant. The difference is mainly driven by cardiac death. POCE was significantly higher in patients with CHF (25.9%) than in patients without CHF (14.0%, P=0.03). This difference is mainly driven by death from all causes.
Discussion
The present study reports on the long-term safety and efficacy of Nobori DES in patients with DM. The main findings at 2-year follow-up are: 1) compared with patients without DM, those with DM had significantly more adverse events and a higher rate of TLF (P=0.006); 2) the presence of IDDM was also associated with significantly higher rate of all composite endpoints (POCE; P=0.006) than NIDDM; 3) the rates of stent thrombosis were low and similar between patients with and without DM, and insulin therapy did not increase the incidence of thrombotic events; and 4) no late or very late stent thromboses occurred in patients with IDDM. Overall, our results confirm that patients with DM, and especially those with IDDM, are at higher risk of adverse events following PCI. They also demonstrate the good performance of the Nobori DES system in this high-risk patient population.
The clinical benefits of Nobori stent implantation have been demonstrated in previous studies.12–14 This is the first study specifically assessing its performance in patients with DM. As expected, patients with DM had worse outcomes than those without DM. The presence of DM was associated with significantly higher 2-year rates of TLF (7.2% vs 4.2%), TLR (4.2% vs 2.5%) and TVR (5.9% vs 3.7%). Compared with other DES, these rates appear lower than those previously reported in studies of sirolimus- and paclitaxel-eluting stents,7,17–20 and they compare favorably with the results of new generations of DES.20–23 For example, patients with DM enrolled in the SPIRIT IV trial who received an everolimus-eluting stent had a 1-year TLF rate of 6.4%.21 In the recently published pooled analysis of SPIRIT and COMPARE trials, patients with DM, treated with Xience V™ stents, had 2-year MACE (major adverse cardiac events: composite of cardiac death, MI, and TLR) rate of 10.1%, and those treated with a Taxus™ stent had a 10.3% 2-year MACE.20
It is well known that patients with DM are at higher risk of adverse events following PCI, especially so for those whose diabetic state is insulin-dependent.1–4 Moreover, IDDM was an independent predictor for late cardiac events and TLR in particular (odds ratio 2.05, P=0.0002).4 In our patient population, IDDM was associated with a 2.0-fold increase in the 2-year rate of TLF. This was driven by significant increases in the rates of TLR, while the rates of cardiac death and MI remained similar between groups. TVR rate was also significantly increased. These higher rates of repeat revascularization procedures are suggestive of an increased incidence of restenosis or the development of new lesions (in previously treated vessels or in vessels remote from the target site), due to the progression of atherosclerosis. Furthermore, complete revascularization was more frequent in non-DM patients as compared to DM patients (the difference between detected and treated lesions was lower in non-DM patients); this pattern certainly could have an impact on TVR in particular. The mean lesion length in patients with diabetes was shorter than in patients without diabetes, contradicting the current understanding of disease pattern in former patients. However, this finding could also indicate that operators tended to apply more spot stent techniques in diffuse disease, potentially leading to higher in-segment revascularization due to disease progression in diabetic patients.
The increased incidence of stent thrombosis reported following DES implantation has been a cause for concern.24,25 This is especially worrisome for patients with DM, as the disease is associated with a pro-thrombotic state and also because they are known to be less responsive to antiplatelet therapy.10,26 At 2-year follow-up, in our study, the rates of stent thrombosis (definite and probable) were low and similar between patients with (1.0%) and without DM (0.7%), and the majority of events occurred within 30 days of the index procedure. Compared with the rates reported in various studies with different stent platforms, the Nobori DES appears to be less thrombogenic than sirolimus- (3.0% to 4.4%),7,17,18 paclitaxel- (2.0% to 2.4%),18,20,22 zotarolimus- (5.6%),22 and everolimus-eluting stents (1.6%).20 Noteworthy is the fact that patients with IDDM were not at higher risk of thrombotic events (0.9% for IDDM vs 1.0% for NIDDM), with no cases of late or very late stent thrombosis having potential clinical relevance. At this stage, it can only be speculated that Nobori DES design and biodegradable polymer might have an impact on this finding.
Our study has several limitations. First, the diagnosis of DM was performed only on the bases of medical history without any confirmatory tests, potentially leading to lower incidence. Furthermore, NOBORI 2 is the non-randomized registry and the comparison with other DES is limited to literature data. Also, under-reporting of adverse events during follow-up is possible. However, because of the very high follow-up compliance rate and meticulous online and on-site source data verification, we believe that most of the adverse events were reported by the investigators, detected during on-site monitoring, or triggered from the database. The 2-year follow-up analysis cannot completely confirm the safety of the stent in this high-risk patient population. The planned 5-year follow-up will therefore be of significant interest.
Conclusion
This analysis of the 2-year outcomes in patients with DM suggests that the Nobori DES is a suitable treatment option for this subset of patients. The absence of late and very late stent thrombosis in IDDM patients merits further investigation, as this finding might have significant clinical value.
Acknowledgment
Funding for the study was provided by Terumo Corporation, Tokyo, Japan.
Disclosure
No author has any conflict of interest to declare in relation to this paper, except being investigators in the NOBORI 2 study.
References
Stein B, Weintraub WS, Gebhart SP, et al. Influence of diabetes mellitus on early and late outcome after percutaneous transluminal coronary angioplasty. Circulation. 1995;91(4):979–989. | |
Elezi S, Kastrati A, Pache J, et al. Diabetes mellitus and the clinical and angiographic outcome after coronary stent placement. J Am Coll Cardiol. 1998;32(7):1866–1873. | |
Carrozza JP Jr, Kuntz RE, Fishman RF, Baim DS. Restenosis after arterial injury caused by coronary stenting in patients with diabetes mellitus. Ann Intern Med. 1993;118(5):344–349. | |
Abizaid A, Kornowski R, Mintz GS, et al. The influence of diabetes mellitus on acute and late clinical outcomes following coronary stent implantation. J Am Coll Cardiol. 1998;32(3):584–589. | |
Moussa I, Leon MB, Baim DS, et al. Impact of sirolimus-eluting stents on outcome in diabetic patients: a SIRIUS (SIRolImUS-coated Bx Velocity balloon-expandable stent in the treatment of patients with de novo coronary artery lesions) substudy. Circulation. 2004;109(19):2273–2278. | |
Dibra A, Kastrati A, Mehilli J, et al; ISAR-DIABETES Study Investigators. Paclitaxel-eluting or sirolimus-eluting stents to prevent restenosis in diabetic patients. N Engl J Med. 2005;353(7):663–670. | |
Jiménez-Quevedo P, Sabaté M, Angiolillo DJ, et al; DIABETES Investigators. Long-term clinical benefit of sirolimus-eluting stent implantation in diabetic patients with de novo coronary stenoses: long-term results of the DIABETES trial. Eur Heart J. 2007;28(16):1946–1952. | |
Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126–2130. | |
Virmani R, Guagliumi G, Farb A, et al. Localized hypersensitivity and late coronary thrombosis secondary to a sirolimus-eluting stent: should we be cautious? Circulation. 2004;109(6):701–705. | |
Joner M, Finn AV, Farb A, et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol. 2006;48(1):193–202. | |
Moreno PR, Fuster V. New aspects in the pathogenesis of diabetic atherothrombosis. J Am Coll Cardiol. 2004;44(12):2293–2300. | |
Danzi GB, Chevalier B, Ostojic M. Nobori™ drug eluting stent system: clinical evidence update. Minerva Cardioangiol. 2010;58(5):599–610. | |
Chevalier B, Silber S, Park SJ, et al; NOBORI 1 Clinical Investigators. Randomized comparison of the Nobori Biolimus A9-eluting coronary stent with the Taxus Liberté paclitaxel-eluting coronary stent in patients with stenosis in native coronary arteries: the NOBORI 1 trial – Phase 2. Circ Cardiovasc Interv. 2009;2(3):188–195. | |
Kadota K, Muramatsu T, Iwabuchi M, et al. Randomized comparison of the Nobori biolimus A9-eluting stent with the sirolimus-eluting stent in patients with stenosis in native coronary arteries. Catheter Cardiovasc Interv. 2012;80(5):789–796. | |
Kumar R, Lee TT, Jeremias A, et al. Comparison of outcomes using sirolimus-eluting stenting in diabetic versus nondiabetic patients with comparison of insulin versus non-insulin therapy in the diabetic patients. Am J Cardiol. 2007;100(8):1187–1191. | |
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40(5):373–383. | |
Ortolani P, Ardissino D, Cavallini C, et al. Effect of sirolimus-eluting stent in diabetic patients with small coronary arteries (a SES-SMART substudy). Am J Cardiol. 2005;96(10):1393–1398. | |
Daemen J, Garcia-Garcia HM, Kukreja N, et al. The long-term value of sirolimus- and paclitaxel-eluting stents over bare metal stents in patients with diabetes mellitus. Eur Heart J. 2007;28(1):26–32. | |
Weber FD, Schneider H, Wiemer M, et al. Sirolimus eluting stent (Cypher) in patients with diabetes mellitus: results from the German Cypher Stent Registry. Clin Res Cardiol. 2008;97(2):105–109. | |
Stone GW, Kedhi E, Kereiakes DJ, et al. Differential clinical responses to everolimus-eluting and paclitaxel-eluting coronary stents in patients with and without diabetes mellitus. Circulation. 2011;124(8):893–900. | |
Kereiakes DJ, Cutlip DE, Applegate RJ, et al. Outcomes in diabetic and nondiabetic patients treated with everolimus- or paclitaxel-eluting stents: results from the SPIRIT IV clinical trial (Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System). J Am Coll Cardiol. 2010;56(25):2084–2089. | |
Chong E, Poh KK, Liang S, Hou XM, Tan HC. Eighteen-month clinical safety and efficacy outcomes of sirolimus-, paclitaxel- and zotarolimus-drug eluting stents in diabetic patients undergoing percutaneous coronary intervention for complex coronary artery stenosis. Ann Acad Med Singapore. 2010;39(5):381–384. | |
Jain AK, Lotan C, Meredith IT, et al; E-Five Registry Investigators. Twelve-month outcomes in patients with diabetes implanted with a zotarolimus-eluting stent: results from the E-Five Registry. Heart. 2010;96(11):848–853. | |
Nordmann AJ, Briel M, Bucher HC. Mortality in randomized controlled trials comparing drug-eluting vs bare-metal stents in coronary artery disease: a meta-analysis. Eur Heart J. 2006;27(23):2784–2814. | |
Camenzind E, Steg PG, Wijns W. Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation. 2007;115(11):1440–1455. | |
Angiolillo DJ. Antiplatelet therapy in type 2 diabetes mellitus. Curr Opin Endocrinol Diabetes Obes. 2007;14(2):124–131. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.