Back to Journals » Clinical Ophthalmology » Volume 13
Does Topical Proparacaine Improve Postoperative Comfort After Strabismus Surgery?
Received 10 September 2019
Accepted for publication 6 November 2019
Published 20 November 2019 Volume 2019:13 Pages 2279—2283
DOI https://doi.org/10.2147/OPTH.S230498
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Robert W Arnold,1 Aleah N Bond2
1Pediatric Ophthalmology and Strabismus, Alaska Children’s EYE & Strabismus, Anchorage, AK 99508, USA; 2Department of Anesthesiology, Wake Forest Baptist Medical Center, Winston-Salem, NC 27101, USA
Correspondence: Robert W Arnold
Pediatric Ophthalmology and Strabismus, Alaska Children’s EYE & Strabismus Address 3500 Latouche #280, AK 99508 Tel +1 907561-1917
Fax +1 907563-5373
Email [email protected]
Background: Strabismus surgery is often performed on children and adults as a quick-turnover, outpatient procedure under general anesthesia. Ideal methods to reduce post-operative pain and nausea are not yet perfected. We postulated that a simple topical anesthetic drop after surgery might help.
Methods: In a prospective study of oculocardiac reflex (OCR) and strabismus surgery, a cohort of ongoing patients either received proparacaine immediately post-op, or none. Co-variables were Intraoperative opioid and OCR, patient age, type of surgery. Several post-operative recovery outcome variables were prospectively monitored.
Results: Sixty strabismus surgery patients (age 15±22 years) received proparacaine 1% while another 80 (16.5±22 years) received none; both received topical antibiotic-steroid ointment. Pain and nausea (Likert scale) were not impacted by covariables complexity of case, age less than 3.5, OCR >33% drop, intraoperative opioid or neuro-status. Immediate post-op heart rate was lower if OCR >33% and if opioids used. Time until discharge was shorter in younger patients. Proparacaine did not impact outcome variables, except in patients younger than 3.5 years when post-op pain was worse.
Conclusion: Post-op topical anesthetic either produced no difference, or worsened post-op pain and recovery. This prospective study does not support the use of topical anesthetic drop to reduce post-strabismus pain and nausea.
Clinical trials registration: NCT03672435, Strabismus Recovery With Proparacaine and Oculocardiac Reflex (OCRprop).
Keywords: oculocardiac reflex, nausea and vomiting, anesthesia recovery, topical anesthetic
Introduction
The trigemino-cardiac reflex (TCR) has afferent orbital stimuli through the fifth cranial nerve with efferent cardiac and gastric vagal stimulation.1 Strabismus surgery stimulates ocular and orbital nociceptors and extraocular muscle proprioceptors. Post-operative pain and nausea (PONV) are common after strabismus surgery. The oculocardiac reflex (OCR) can arise from various orbital stimuli including globe pressure, but is typically generated by intra-operative tension-dependent traction on an extraocular muscle.2
Surgeons and anesthesiologists have tried to reduce adverse post-operative and intraoperative neurologic sequelae from strabismus surgery.3 Pre-operative sub-tenons block did not provide superior post-op pain relief compared to intraoperative fentanyl but OCR was more common with fentanyl.4 Other authors, however, concluded that subtenons injection may reduce post-strabismus pain and nausea.5–7 Post-strabismus injection of lidocaine sub-Tenons had less post-operative agitation than sub-tenons saline injection.8
Orbital pressure and pain can cause prolonged oculocardiac reflex.9,10 While serum gastrin was not markedly increased in a small number of oculocardiac reflex patients,11 it is not clear whether patients with more intraoperative vagal stimulation have more post-operative pain, nausea and vomiting. Therefore, the role of immediate post-operative topical pain relief in strabismus patients is not clear.
One 2003 study addressed the impact of topical anesthesia on post-strabismus pain. Topical amethocaine 0.5% and ketorolac 0.5% before and at the end of general anesthesia for simple bilateral rectus recession were similar to placebo regarding post-operative pain in younger children.12 We thought this previous topical anesthesia study that randomized 51 younger children with simple recession surgery into three groups may have been under-powered. With a standard deviation of 2, alpha of 0.05 and power of 0.8, this study might have been powered to detect a 100% difference in pain scores (i.e. from 2±2 to 4±2). We suspected pain was greater in more complex strabismus cases and in older patients. Therefore, we sought to detect half the difference with a sample size of >63 per group. We prospectively monitored intraoperative oculocardiac reflex and post-operative pain and nausea in response to one drop of proparacaine 1% added to post-operative antibiotic-steroid ointment applied after strabismus surgery.
Methods
In an ongoing prospective oculocardiac reflex study with timely institutional review board approval from Providence Hospital (Anchorage, Alaska), patients undergoing strabismus surgery routinely had oculocardiac reflex monitored during 10 s, 200 g, square-wave traction on an extraocular rectus muscle. This observational study of routine anesthesia care did not require signed consent. Due to inter-rectus muscle variability, and for practical access, the inferior rectus muscle was most frequently tested. Intraoperative opioid use and anesthetic agents, at the preference of the anesthesiologist and independent of topical therapy, were recorded. None of these patients received dexmedetomidine.13 Following each strabismus case, antibiotic-steroid ointment (neomycin sulfate, polymixin-B dexamethasone, Alcon, Ft. Worth and generics) was instilled in operative eyes. Patients on some days received topical anesthetic post-operatively; this was known only to the operating room staff and not the recovery staff. Proparacaine 1% (Alcaine, Alcon, Ft. Worth) was instilled in this portion of cases before ointment was instilled.
During the strabismus surgery, oculocardiac reflex was prospectively monitored utilizing a predefined protocol; electrocardiograph was monitored during 10 s, 200 g, square-wave traction on an extraocular rectus muscle. Due to inter-rectus muscle variability, and for practical access, the inferior rectus muscle was most frequently tested if the conjunctival incision for planned muscle afforded access to the inferior rectus. OCR is expressed as a percent drop from stable baseline heart rate.
The post-operative nursing staff then collected data on each patient’s recovery which was later analyzed with respect to proparacaine plus ointment vs ointment alone. The recovery process was two-stage with initial intense nursing monitoring (stage 1) followed by routine care in preparation for discharge (stage 2). Data collected were heart rate, blood pressure, pain (Likert scale 10 range14), irritability, nausea/vomiting (episodes), methods to alleviate pain and agitation in immediate recovery and second stage, and time-to-discharge. The type of strabismus procedure was categorized as simple (rectus muscle virgin recessions and/or inferior oblique myectomy) and complex (recess-resect procedures, re-operations, transpositions, superior oblique). The neurologic status of patients was recorded as “normal” or not normal (Down syndrome, cerebral palsy, traumatic brain injury, epilepsy, neurodevelopmental delays).
Results
A total of 140 patients were randomized; 60 to receive ointment plus proparacaine after strabismus surgery while 80 received ointment alone. The groups age did not differ (proparacaine plus ointment (15.0 ±6 years) versus ointment alone (16.6±5) (unpaired, two-sample Student's t-test, p = 0.652). The cohorts were similar; those who received proparacaine compared to those who did not: the proportion of complex cases was 38% versus 41%, use of opioids was 45% versus 40%, and presence of neurological disorders was 7% compared to 10%. The average ± standard deviation OCR was −22±18% for proparacaine cases versus −20±18% in cases with no proparacaine. Heart rate in recovery was not different in the group receiving proparacaine versus those who did not (t-test, p = 0.576). Pain score on entry to recovery was also not different when proparacaine was given (Mann–Whitney, p = 0.472). Post-operative nausea and vomiting did not differ whether proparacaine was given (Mann–Whitney, p = 0.391). Additional interactions between variables are given in Table 1. Heart rate on entry to recovery was lower in patients who had been given opioids, on patients with more oculocardiac reflex, and was higher in children younger than 3.5 years.
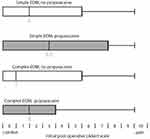
Comparing the 56 complex cases with the 84 simple strabismus cases, with or without proparacaine, age averaged 21±26 years versus 12±18 years, and OCR was −20±18% versus −21±18%. Pain entering recovery averaged 2.9±3.6 versus 3.5.±3.6 while pain in stage 2 decreased to 2.7±2.8 and 1.8±2.4 for simple cases on the 10-point Likert scale. The pain entering recovery was not different based on the complexity of procedure (Mann–Whitney, p = 0.298). Heart rate entering recovery did not differ based on procedure complexity (t-Test, p=0.609). There was no difference in post-operative nausea and vomiting based on procedure complexity (Mann–Whitney, p = 0.148). The lack of impact of proparacaine versus no proparacaine in simple and complex strabismus cases is illustrated in Figure 1.
With proparacaine administration as a co-variable, no other variable had significant impact other than patients in the age cohort less than 3.5 years had more post-operative pain (Mann–Whitney, P=0.02). The 17 younger children given proparacaine had pain scales 6.2±4.3 while the 19 given antibiotic ointment alone had pain scores 2.3±3.9.
In this group of patients, the percent oculocardiac reflex was greater in younger patients (%OCR = −0.002 (age) + 24.5%, r(138) = 0.27, p < 0.01).
Conclusion
In this prospective, single-blind study, adding proparacaine to antibiotic-steroid ointment at the conclusion of a strabismus case produced no improvement in post-operative pain, irritability or time to discharge, and may have been worse for younger children.
We are not sure why the postoperative pain scores in younger children who received proparacaine were worse than those who did not. We did not want corneal desiccation associated with anesthetic corneas and lagophthalmos so we were careful to instill adequate antibiotic-steroid ointment in all operative eyes. Further investigation may be indicated, but we have decided against routine topical anesthesia following strabismus surgery for all ages.
We pondered whether complex cases involving more extensive dissection and tension on extraocular muscles might lead to more post-operative irritation, but this study was not of sufficient power to detect that. Adding proparacaine to the antibiotic ointment did not afford any advantage for patients whether they had simple, or complex types of strabismus procedures.
Topical anesthetics have a profound impact on the cornea with the duration of action 10–15 mins. The impact of topical anesthesia on conjunctiva or the deeper structures Tenon’s capsule or extraocular muscle may be substantially less, and be of shorter duration due to vascularity of tissue and penetration of the drop.
Post-operative nausea and pain were not related to intraoperative oculocardiac reflex in our series – similar to observations in adults,15 but differing from a study in children.16 In some of our prior studies,17,18 we found more oculocardiac reflex in younger patients, however another recent study on anesthetic depth19 and this current study shows slightly more percent oculocardiac reflex in younger patients. We also observed lower recovery room heart rates in patients who received intra-operative opioids. Whether this impact on oculocardiac reflex is related to pre-operative oral sedation – in the younger patients – or related to opioid, is the topic of our further study.
Data Sharing Statement
Deidentified data: http://www.abcd-vision.org/OCR/OCR proparacaine de-identified.pdf.
Disclosure
Dr. Arnold is a board member of Glacier Medical Software that markets ROP-Check NICU software and of PDI Check, LLC that markets PDI Check near vision game for the Nintendo 3DS. Dr Arnold reports non-financial support from Glacier Medical Software, non-financial support from PDI Check, non-financial support from Alaska Blind Child Discovery, outside the submitted work. In addition, Dr Arnold has a patent PDI Check pending to Robert Arnold and Alex Damarjian; and Protocol Developer and Investigator for the Pediatric Eye Disease Investigator Group (PEDIG); Non-paid advisory board for GoCheck Kids, PlusoptiX, iScreen, Adaptica. The authors report no other conflicts of interest in this work.
References
1. Meuwly C, Chowdhury T, Sandu N, et al. Definition and diagnosis of the trigeminocardiac reflex: a grounded theory approach for an update. Front Neurol. 2017;8:533. doi:10.3389/fneur.2017.00533
2. Machida CJ, Arnold RW. The effect of induced muscle tension and fatigue on the oculocardiac reflex. Binoc Vis and Strabismus Quart. 2003;18(2):81–86.
3. Stowman AM, Bothun ED, Belani KG. Discomfort, delirium, and PONV in infants and young children undergoing strabismus surgery. Minn Med. 2011;94(3):39–41.
4. Ramachandran R, Rewari V, Chandralekha C, Sinha R, Trikha A, Sharma P. Sub-tenon block does not provide superior postoperative analgesia vs intravenous fentanyl in pediatric squint surgery. Eur J Ophthalmol. 2014;24(5):643–649. doi:10.5301/ejo.5000438
5. Gupta N, Kumar R, Kumar S, Sehgal R, Sharma KR. A prospective randomised double blind study to evaluate the effect of peribulbar block or topical application of local anaesthesia combined with general anaesthesia on intra-operative and postoperative complications during paediatric strabismus surgery. Anaesthesia. 2007;62(11):1110–1113. doi:10.1111/ana.2007.62.issue-11
6. Ibrahim AN, Shabana T. Sub-Tenon’s injection versus paracetamol in pediatric strabismus surgery. Saudi J Anaesth. 2017;11(1):72–76. doi:10.4103/1658-354X.197349
7. Steib A, Karcenty A, Calache E, Franckhauser J, Dupeyron JP, Speeg-Schatz C. Effects of subtenon anesthesia combined with general anesthesia on perioperative analgesic requirements in pediatric strabismus surgery. Reg Anesth Pain Med. 2005;30(5):478–483. doi:10.1097/00115550-200509000-00010
8. Seo IS, Seong CR, Jung G, Park SJ, Kim SY, Kim MM. The effect of sub-tenon lidocaine injection on emergence agitation after general anaesthesia in paediatric strabismus surgery. Eur J Anaesthesiol. 2011;28(5):334–339. doi:10.1097/EJA.0b013e3283426ed6
9. Westerling D, Blohme J, Stigmar G. Orbital mass in a child causing somnolence, nausea and bradycardia. Can J Anaesth. 1998;45(8):777–780. doi:10.1007/BF03012148
10. Negrutiu S, Pop R, Cardan E. Reflex oculocardiac persistent consecutiv unui hematom retrobulbar. Prezentare de caz. [Persistent oculocardiac reflex following retrobulbar hematoma. Case report]. Rev Chir Oncol Radiol O R L Oftalmol Stomatol Ser Oftalmol. 1988;32(2):149–151.
11. Blanc V, Ruest P, Brisson G, Jacob J-L. Serum gastrin and blood glucose levels during halothane-nitrous oxide anaesthesia and strabismus surgery in children. Can J Anaesth. 1991;38(1):43–48. doi:10.1007/BF03009162
12. Kim J, Azavedo L, Bhananker S, Bonn G, Splinter W. Amethocaine or ketorolac eyedrops provide inadequate analgesia in pediatric strabismus surgery. Can J Anaesth. 2003;50(8):819–823. doi:10.1007/BF03019379
13. Arnold RW, Biggs RE, Beerle BJ. Intravenous dexmedetomidine augments the oculocardiac reflex. J AAPOS. 2018;22(3):211–213.e211. doi:10.1016/j.jaapos.2018.01.016
14. Watcha MF, Medellin E, Lee AD, Felberg MA, Bidani SA. Validation of the pictorial Baxter Retching Faces scale for the measurement of the severity of postoperative nausea in Spanish-speaking children. Br J Anaesth. 2018;121(6):1316–1322. doi:10.1016/j.bja.2018.07.036
15. Tramér M, Fuchs-Buder T, Sansonetti A, Rifat K. Low incidence of the oculocardiac reflex and postoperative nausea and vomiting in adults undergoing strabismus surgery. Can J Anaesth. 1997;44(8):830–835. doi:10.1007/BF03013159
16. Allen L, Sudesh S, Sandramouli S, Cooper G, McFarlane D, Willshaw H. The association between the oculocardiac reflex and post-operative vomiting in children undergoing strabismus surgery. Eye. 1998;12(2):193–196. doi:10.1038/eye.1998.46
17. Stump M, Arnold RW. Iris color alone does not predict susceptibility to the oculocardiac reflex in strabismus surgery. Binocul Vis Strabismus Q. 1999;14(2):111–116.
18. Arnold RW, Jensen PA, Kovtoun TA, Maurer SA, Schultz JA. The profound augmentation of the oculocardiac reflex by fast acting opioids. Binocul Vis Strabismus Q. 2004;19(4):215–222.
19. Arnold RW, Bond AN, McCall M, Lunoe L. The oculocardiac reflex and depth of anesthesia measured by brain wave. BMC Anesthesiol. 2019;19(1):36. doi:10.1186/s12871-019-0712-z
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.