Back to Journals » International Journal of Nanomedicine » Volume 9 » Issue 1
Development of Yersinia pestis F1 antigen-loaded microspheres vaccine against plague
Authors Huang S, Li I, Hong P, Yeh M
Received 19 October 2013
Accepted for publication 12 December 2013
Published 7 February 2014 Volume 2014:9(1) Pages 813—822
DOI https://doi.org/10.2147/IJN.S56260
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Shih-shiung Huang,1 I-Hsun Li,2,3 Po-da Hong,1 Ming-kung Yeh1,2,4
1Biomedical Engineering Program, Graduate Institute of Engineering, Department of Materials Science and Engineering, National Taiwan University of Science and Technology, Taipei, Taiwan, Republic of China; 2School of Pharmacy, 3Department of Pharmacy Practice, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 4Food and Drug Administration, Ministry of Health and Welfare, Taipei, Taiwan, Republic of China
Abstract: Yersinia pestis F1 antigen-loaded poly(DL-lactide-co-glycolide)/polyethylene glycol (PEG) (PLGA/PEG) microspheres were produced using a water-in-oil-in-water emulsion/solvent extraction technique and assayed for their percent yield, entrapment efficiency, surface morphology, particle size, zeta potential, in vitro release properties, and in vivo animal protect efficacy. The Y. pestis F1 antigen-loaded microspheres (mean particle size 3.8 µm) exhibited a high loading capacity (4.5% w/w), yield (85.2%), and entrapment efficiency (38.1%), and presented a controlled in vitro release profile with a low initial burst (18.5%), then continued to release Y. pestis F1 antigen over 70 days. The distribution (%) of Y. pestis F1 on the microspheres surface, outer layer, and core was 3.1%, 28.9%, and 60.7%, respectively. A steady release rate was noticed to be 0.55 µg Y. pestis F1 antigen/mg microspheres/day of Y. pestis F1 antigen release maintained for 42 days. The cumulative release amount at the 1st, 28th, and 42nd days was 8.2, 26.7, and 31.0 µg Y. pestis F1 antigen/mg microspheres, respectively. The 100 times median lethal dose 50% (LD50) of Y. pestis Yokohama-R strain by intraperitoneal injection challenge in mice test, in which mice received one dose of 40 µg F1 antigen content of PLGA/PEG microspheres, F1 antigen in Al(OH)3, and in comparison with F1 antigen in Al(OH)3 vaccine in two doses, was evaluated after given by subcutaneous immunization of BALB/c mice. The study results show that the greatest survival was observed in the group of mice immunized with one dose of F1 antigen-loaded PLGA/PEG microspheres, and two doses of F1 antigen in Al(OH)3 vaccine (100%). In vivo vaccination studies also demonstrated that F1 vaccines microspheres had a protective ability; its steady-state IgG immune protection in mice plasma dramatic increased from 2 weeks (18,764±3,124) to 7 weeks (126,468±19,176) after vaccination. These findings strongly suggest that F1-antigen loaded microspheres vaccine offer a new therapeutic strategy in optimizing the vaccine incorporation and delivery properties of these potential vaccine targeting carriers.
Keywords: PLGA, immunological, protective responses
Introduction
Yersinia pestis is a Gram-negative bacterium and the causative agent of plague. In man, plague can occur in three forms: bubonic, septicemic, and pneumonic. Bubonic plague arises following transmission by flea vectors, causing the swelling of lymph nodes in the victim, typically in the axillae or groin to form buboes. If detected in time, this infection is susceptible to intensive antibiotic therapy and individuals should recover. Occasionally, septicemic plague infection can occur without the appearance of buboes; this is a more insidious presentation, providing fewer triggers-to-treat and a vague general syndrome. Pneumonic plague can develop as a secondary syndrome in infected individuals or else can develop as a primary infection following exposure to an aerosol of Y. pestis organisms from an infected individual in close contact. In the first decade of the 21st century, 56 persons were reported to have the disease in the United States, of which seven died. Worldwide, 21,725 persons were affected, with 1,612 deaths, for a case-fatality rate of 7.4%.1
Vaccines against bubonic plague have been available as killed whole-cell preparations since the mid-19th century and generally have been demonstrated efficacious against the bubonic form of the disease.2–4 Protecting against the pneumonic form of the disease has been possible only with live attenuated strains of Y. pestis.5 Subunit antigens of Y. pestis were identified as long ago as the mid-twentieth century,3–9 but it was only with the advent of recombinant DNA technology that these could be fully exploited with consistent production of pure, stable recombinant proteins.6,7,10–12
The field of nanotechnology has growing applicability to medical biotechnology, including drug and vaccine delivery.9,13–17 Polymeric particles made from inert materials or biodegradable polymers such as poly-l-lactide (PLA)18,19 or poly-l-lactide-co-glycolides (PLGAs)20–23 allow drug encapsulation within a hydrophobic core or absorption to the hydrophilic shell.23,24 This encapsulation processes can be manipulated to encapsulate drugs or vaccines within the interior.25,26 Particles of different sizes might influence the immune response to the passenger antigen.27
Here we describe the encapsulation of Y. pestis F1-antigen onto PLGA/PEG microspheres in order to determine whether this delivery system will enhance immunogenicity in mice. The size of microspheres, encapsulation efficiency, in vitro release profiles, and release pattern were reported. The formulation was further evaluated for in vivo animal protect efficacy. The goal of the study is developed Y. pestis F1 antigen-loaded PLGA/PEG microspheres, which might enhance the efficiency of the Y. pestis F1 antigen (adjuvant effect) while conferring long-term protection. The ultimate aim was to produce an effective, single-dose formulation based on the currently used vaccines.
Methods
Materials
Y. pestis F1, the Fl antigen, was purified from the culture supernate of Y. pestis grown at 37°C in BHI broth medium (Difco, Detroit, MI, USA). The F1 was extracted by 30% ammonium sulfate precipitation overnight at 4°C, collected the protein by centrifugation, and resuspended in 0.1 × volume of phosphate-buffered saline (PBS), 30% ammonium sulfate precipitation overnight at 4°C again. The protein was collected by centrifugation and resuspended in 0.05 × volume of water, and dialyzed against water, analyzed by SDS-PAGE, then freeze-dried and weighed. PLGA 50:50 was obtained from Boehringer Ingelheim (Ingelheim, Germany), Resomer RG 502 (molecular weight [Mw]: 12,000; inherent viscosity: 0.24 dL/g). Bicinchoninic acid solution (BCA), copper (II) sulfate, sodium dodecyl sulfate (SDS) and PBS were obtained from Sigma-Aldrich (St Louis, MO, USA). Polyethylene glycol (PEG) (Mw 6,000), poly(vinyl pyrrolidone) (PVP) (Mw 40,000) were obtained from Sigma-Aldrich. Dichloromethane (DCM), acetone, tetrahydrofuran and methanol were supplied by BDH (Poole, UK). All materials were used as supplied.
Characterization of protein integrity
Preparation of microspheres
The preparation of microspheres was conducted using minor modifications of a previously published water-in-oil-in-water (w/o/w) solvent evaporation method.19,28 Briefly, 30 mg Y. pestis F1 in 1 mL PBS buffer was added to 5 mL of DCM containing 300 mg PLGA/PEG 2:1 using a homogenizer (20,000 rpm for 3 minutes) to provide the primary emulsion. The resulting emulsion was then mixed at high speed with 30 mL of continuous phase solution containing 10% (w/v) PVP as an emulsion stabilizer. The resulting w/o/w multiple emulsion was stirred with a magnetic stirrer for 16 hours under ambient conditions to extract DCM. The microspheres were cleaned by centrifugation and resuspension in distilled water three times to remove PVP and were then freeze-dried. The final products were stored in desiccators below 4°C. At least three lots of microspheres were prepared for each formulation. The production yield was calculated by the following equation:
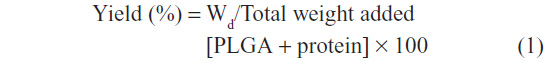
where Wd is the weight of dry microspheres.
Determination of Y. pestis F1 loading of microspheres
Accurately weighed 8–10 mg of freeze-dried microspheres were treated with 1 mL of acetone and shaken for 2 minutes at 120 rpm.29 The sample was centrifuged. BCA assay was used to determine the F1 concentration in the supernatant against a series of F1 standards obtained from placebo microspheres treated under the same conditions. Each sample was assayed in triplicate.
The entrapment% (E%) and encapsulation efficiency (EE%) of protein were calculated from the equation indicated below:30
where Wt is the determination of protein amount, Wm is the weight of microspheres, and Wi is the initial added amount of protein.
Distribution of F1
Analysis of surface protein
The amount of protein associated with the surface of protein-loaded microspheres was estimated using two approaches for comparison as described previously.31
Treatment with BCA reagent
The analysis of surface protein by BCA is based on the displacement of adsorbed proteins by a negatively charged detergent that binds to hydrophobic regions of protein molecules, causing them to unfold into extended polypeptide chains and freeing them from association with other molecules. Microspheres (5–6 mg) were suspended in 0.5 mL PBS and mixed with BCA reagent (2 mL BCA solution, 40 mL copper [II] sulfate). The samples were shaken for 2 minutes at room temperature. The microspheres were sedimented by centrifuging and the supernatant was analyzed for protein content using the BCA procedure. At least three samples of microspheres were assayed for each formulation.
Treatment with 2% SDS
The above sedimented sample were redispersed in 1 mL of 2% (w/v) SDS solution and agitated for 4 hours at room temperature using an IKA Vibrax shaker (Sigma-Aldrich). The samples were centrifuged at 4,000 g for 5 minutes and the supernatant was analyzed for protein using a BCA assay. At least three samples of microspheres were assayed for each formulation. The analysis of weak binding protein by 2% SDS is based on proteins binding to PLGA microspheres, causing them to digest into extended polypeptide chains and freeing them from association with by PLGA.
Treatment with 5% SDS
The analysis of reserved protein by 5% SDS is based on the PLGA microspheres digest into polypeptide chains and frees them from association with by PLGA. The above sedimented sample were redispersed in 1 mL of 5% (w/v) SDS solution and agitated for 16 hours at room temperature using an IKA Vibrax shaker. The samples were centrifuged at 4,000 g for 5 minutes and the supernatant was analyzed for protein using a BCA assay. At least three samples of microspheres were assayed for each formulation.
Particle size
Particles were ultrasonicated to produce well-dispersed microspheres in deionized water and measured using a dynamic light-scattering particle-size analyzer (LB-500, Horiba, Kyoto, Japan). Average particle size was expressed as volume mean diameter in μm. Each sample was analyzed in triplicate.
Zeta potential
Microspheres were dispersed in deionized water using an ultrasonicater. The particle zeta potential was recorded using ZetaPlus (Brookhaven Instruments Corporation, Holtsville, NY, USA). Each sample was analyzed at least five times to give an average value and standard deviation for particle zeta potential.
Microsphere morphology
The microspheres were characterized by scanning electron microscopy (SEM) using an AMR1000. Samples were mounted on a carbon adhesive tab and sputter coated (10–15 nm) with gold palladium (60/40 alloy).
In vitro Y. pestis F1 release from microspheres28
A series of tubes containing triplicate microsphere samples (5 mg) was suspended in 1 mL of sterile-filtered buffer (100 mM sodium phosphate, 10 mM sodium chloride, 0.03% polysorbate 80, pH 7.4), then incubated at 37°C under static conditions for 0.25, 1, 2, 3, 4, 7, 14, 21, 28, 35, 42, 56, 63, and 70 days. The samples were then centrifuged (4 minutes; 17,500 g). The release medium was replaced with a fresh buffer. Filtered (0.2 μm low-protein-binding Aerodisk HT) samples were assayed using the BCA method. The pH of the medium was confirmed to be 7.2±0.2 through the study duration. Unreleased protein was recovered by extraction of the remaining microsphere mass as described above. All protein quantities are expressed as a percentage of the initial protein present based on the theoretical load and the initial microsphere mass.
Animal study
Immunization and challenge experiments in mice
Studies in laboratory animals were designed and conducted in AAALAC-accredited animal facilities in accordance with the regulations and guidelines of the National Science Animal Centre, Taiwan, Republic of China. The mice were housed in pairs in polypropylene cages, with free access to food and water. The vivarium was maintained on a 12-hour light:12-hour dark cycle, with a room temperature of 22°C±1°C and relative humidity level of 50%±5%. All studies were in compliance with the rules set forth in the Guide for the Care and Use of Laboratory Animals. Animal immunization and challenge experiments were adapted from previous report.31–33 In brief, for challenge experiments, the BALB/c inbred strain mice were purchased from National Laboratory Animal Facility, National Science Council, Taipei, Taiwan, Republic of China, and were housed at Animal Facility of National Defense Medical Center under barrier condition.
The characteristics of the F1-loaded PLGA/PEG microspheres used for immunization are presented in Table 1. For immunization experiments, each group of ten mice were immunized. In the protection experiments, on Day 0, a PBS solution as control (group A), a 40 μg dose of Fl antigen encapsulated in 0.1 mL PLGA/PEG microspheres (group B), and Fl antigen in Al(OH)3 (group C) were given subcutaneously in a single dose to groups of ten mice. Two 40 μg doses of Fl antigen in Al(OH)3 (group D) were administered subcutaneously to the mice on Days 0 and 16. Following administration, body mass, and food intake were measured weekly.
To test the efficacy of the F1 antigen vaccines, immunized mice were challenged with Y. pestis Yokohama-R L00702 100 times the median lethal dose 50% (LD50) (103 colony-forming units) by intraperitoneal injection at 45 days after the first immunization. All mouse care and procedures were in accordance with institutional policies for animal health and well-being, and all challenges adhered to Biosafety Level 3 practices. Mice morbidity rate and survival rate were monitored daily for 10 days after challenge for development of symptoms. Animals that succumbed to challenge were autopsied, livers and spleens were scored for enlargement, and any evidence of abnormality was noted. The immune response of anti-F1 IgG antibody titer was also determined in BALB/c mice. Serum was collected at Week 5.
Immunoanalysis
For the bioactivity studies, the containing F1 antigens were coated in the micro-enzyme-linked immunoassay (ELISA) plate and the anti-F1 IgG antibody titer was evaluated using antigen-specific antibodies and analyzed by ELISA. Briefly, 96-well microtiter plates were coated with F1 antigens diluted to 5 μg/mL in PBS buffer (pH 9.6) and incubated overnight at 4°C. Nonspecific binding was blocked with 1% BSA in PBS buffer. Pooled test sera were diluted in twofold serial dilutions across the plates and incubated at 37°C for 1 hour. After five washes by 0.01 M PBS buffer containing 0.05% Tween-20 (PBST), horseradish peroxidase-labeled goat antimouse IgG (Roche, Basel, Switzerland) diluted 1:1000 in PBST was added to each well and incubated for 30 minutes at 37°C. The plates were washed three times in PBST buffer, and 100 μl of 0.01% peroxidase substrate 3,3′,5,5′-tetramethylbenzidine (Kirkegaard and Perry Laboratories, Gaithersburg, MD, USA) was added to each well. The reaction was stopped by the addition of 50 μl of 2.5 M H2SO4 per well, and then optical density was read at 450 nm with an ELISA plate reader (Bio-Rad, Hercules, CA, USA). Titers were expressed as the reciprocal of the dilution that intercepted the baseline (mean of negative control well plus three standard deviation).
Cytokine level measurement
In order to measure the IFN-γ, TNF-α, and IL-4, sera were collected from the four groups of animals after 35 days of postprimary immunization before challenge with Y. pestis Yokohama-R L00702. The levels of three cytokines IFN-γ, TNF-α, and IL-4 were measured by cytokine-specific BD OptEIATM™ Set (BD Biosciences, San Jose, CA, USA) according to the manufacturer’s instructions. Concentration of specific cytokine was calculated from standard curve and data were presented as mean concentration of cytokine (pg/mL) of triplicate wells.
Statistical analysis
Survival after each treatment was analyzed using Kaplan–Meier survival curves. Nonparametric Kruskial–Wallis statistics were used to determine overall treatment effect using the day of death as the nonparametric variable. The nonparametric modification of the Neuman–Keuls test was used for subsequent pairwise comparisons. The effects of F1-loaded PLGA/PEG microspheres were compared using a one-way analysis of variance. Results were considered statistically significant if P<0.05.
Results and discussion
Characteristics of Y. pestis F1-loaded PLGA/PEG microspheres
The characteristic of Y. pestis F1-loaded PLGA/PEG microspheres presented in Table 1, using the PLGA/PEG 2/1 and adding salt in the primary phase to prepare the Y. pestis F1-loaded microspheres for the delivery of antigens and/or adjuvants. The surface of Y. pestis F1-loaded PLGA/PEG microspheres is characteristically smoothly (Figure 1). There were no substantial variations in terms of surface roughness observed on the surfaces of the particles.
Particles have been shown to traffic to the draining lymph node in a size-dependent manner. An attractive strategy would be to deliver the vaccine-loaded microspheres to a subset of draining lymph nodes corresponding to a specific site or organ to minimize systemic toxicity.8,34 Rao et al22 showed that lymphatic uptake and node retention of particles was inversely related to size and hydrophobicity, and directly related to the anionic charge on the particles. The 50 nm particles were ideal for sustained regional delivery into the lymphatics for prevention/treatment of oligometastases. Florence et al35 already demonstrated that particles uptake was by way of the Peyer’s patches and other elements of the gut-associated lymphoid tissue. Modification of the particle surface with specific ligands has indicated widespread uptake by nongut-associated lymphoid tissue, following their binding to and internalization by enterocytes. In a separate study, carboxylated polystyrene nanoparticles of various sizes, normalized for equal doses of conjugated antigen, were used to study size-dependent immunogenicity. Particle sizes of microspheres play an important role during uptake through the M-cells present in the Peyer’s patches of the intestines and by antigen presenting cells that mediate immune responses. When microspheres of sizes <5 μm extravasate from the Peyer’s patches within macrophages which disseminate into systemic lymphoid tissues, where antigen release would be expected to induce a circulating antibody response.36 Also, large particles (500–2,000 nm) are engulfed by peripheral APCs at the site of injection, while small nanoparticles (20–200 nm) are internalized in macrophages residing in lymph nodes. Smaller nanoparticles were independently able to diffuse across the interstitium and enter the lymphatic system, while delayed transport of larger nanoparticles to lymph nodes supports a requirement for cell-based transport. In contrast, microspheres with sizes higher than 5 μm remain in the IgA inductive environment of the Peyer’s patches, where antigen recognition would stimulate a disseminated mucosal IgA immune response. It has been suggested by many researchers, including Eldridge et al13, that the most attractive possibility of concurrent circulating IgG and secretory IgA immunity is achievable through oral immunization with vaccine-microspheres spanning the size range of 1–10 μm. The size range achieved by this project, therefore, is ideal for maximizing mucosal and systemic immune response. Rosli et al37 demonstrated that the transgene protein expression and IgA antibody responses at local mucosal sites suggest immunological response to a potential oral DNA vaccine formulated within the microsphere carriers. Thomas et al38 reported that the surface charge of microspheres as indicated by the zeta potential has a significant effect on its uptake by phagocytic cells of the immune system. They reported that the further the potential is from zero or greater the absolute value of the zeta potential of the particle, the more effective are their uptake. Zeta potential can also be used as an indicator of the suspension stability. The higher the absolute value, the greater the repulsive forces between the particles; therefore, the potential for coagulation and flocculation is at the minimum. The high zeta potential, therefore, increases the chances of uptake of the microspheres through the Peyer’s patches. Since the goal of this project is to induce immune response to the encapsulated Y. pestis F1 antigens, it is important that the particle sizes and zeta potential of the microspheres are within the range that makes their potential phagocytosis by antigen presenting cells possible. The Y. pestis F1 antigens formulation with zeta potential of −23.8 mV was ideal for vaccine delivery and was chosen for the in vivo studies.
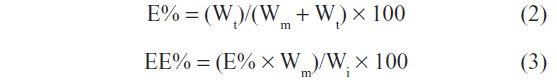
Figure 2 summarizes the findings of in vitro Y. pestis F1 release study. The cumulative release of Y. pestis F1 antigen, in terms of %w/w, provided an index of delivery efficiency; it had an upper limit of 70.4% of the Y. pestis F1 antigen load at 42 days. The initial burst release of Y. pestis F1 microspheres was estimated from the cumulative release of 24 hours to be 16.5%, followed by a sustained diffusion of F1 antigen from the particles. A steady release rate was noticed to be 0.55 μg Y. pestis F1 antigen/mg microspheres/day of Y. pestis F1 antigen release maintained for 42 days. The cumulative release amount at day 1, 28, and 42 was 8.2, 26.7, and 31.0 μg Y. pestis F1 antigen/mg microspheres, respectively. Our Y. pestis F1-loaded microspheres, formulations prepared with a PLGA:PEG ratio of 2:1 with a smaller average diameter, showed the most suitable release pattern among the formulations studied. The cumulative amount of the Y. pestis F1 show the release of the antigen was extended throughout the study period. Continuous release of antigens has been found to be useful, since it leads to continuous exposure to low quantities of antigens. Thus, incorporation of extra amounts of hydrophobic polymer with PEG might have caused more appropriate polymeric networks to deliver the F1 antigen for a prolonged period of time among the experimental formulations. In most of the studies previously described using PLGA microspheres for protein delivery, the protein had been adsorbed onto the surface of microspheres.26,39–43 The most notable aspect of the current studies is the entrapped effect and controlled release effect of potent active Y. pestis F1 antigen achieved through the presentation of Y. pestis F1 inside PLGA/PEG 2:1 microspheres. The Y. pestis F1-loaded microsphere delivery system offers the prospect of achieving a long-term, multiple phase release, single dose vaccine in the future.
  | Figure 2 Cumulative release amount (A) and % (B) of Yersinia pestis F1 antigen from PLGA/PEG 2:1 microspheres. |
Animal study
To assess the efficacy of Y. pestis F1-loaded PLGA/PEG microspheres immunization against Y. pestis infection, the mice were checked daily for survival rates for the differential experimental groups at 10 days postchallenge, and the results are shown in Figure 3A. The greatest survival was observed in the group of mice immunized with 40 μg Y. pestis F1-loaded PLGA/PEG microspheres and two doses of 40 μg Y. pestis F1-loaded Alum, in which ten out of the ten tested mice survived the Y. pestis challenge. The second best survival rate was observed in the group of mice immunized with 40 μg F1 antigen with Alum one dose, whose survival rate was 70%. In contrast, the PBS solution alone group failed to confer a comparable level of protection on the immunized mice. Mice immunized with the F1-loaded microspheres vaccine showed full protection (100% survival). These efficacies were better than those mice immunized with F1-Al(OH)3 one dose only (70% survival; P<0.05). These results suggest that the F1-loaded microspheres vaccine can contribute to protective immunity against plague. Figure 3B show that the Y. pestis F1-specific IgG antibody response elicited by Y. pestis F1 immunization. As shown in Figure 3B, the F1-loaded PLGA/PEG microspheres showed higher specific antibody responses than one dose of F1-Al(OH)3 immunized groups after injections. The F1 vaccines microspheres had a protective ability; its steady-state IgG immune protection in mice plasma dramatically increased from 2 weeks (18,764±3,124) to 7 weeks (126,468±19,176) after vaccination, and this was threefold higher than that observed for one dose of F1 vaccine in Al(OH)3 at 45 days. However, much stronger antibody responses were noticed in Y. pestis F1-loaded microspheres immunized mice after the Y. pestis Yokohama-R strain L00702 challenge, indicating a priming effect of Y. pestis F1-loaded microspheres immunization in an antigen-specific manner. Mice morbidity was observed; tremors, thicker fur, impatience, weakened activity, poor eating habits, and other signs of illness and death were recorded (Figure 3C). No significantly different body weights were recorded across groups (Figure 3D).
To assess the types of Th cell responses elicited by the F1 antigen vaccines, cytokine responses were measured after 35 days of postprimary immunization by cytokine-specific BD OptEIATM Set. The specific IFN-γ, TNF-α, and IL-4 were significantly enhanced as were IFN-γ, TNF-α, and IL-4, particularly by the F1-loaded microspheres-immunized and F1-Al(OH)3 groups. Figure 4 showed that F1-Al(OH)3 group resulted in higher IL-4 level, and relatively lower IFN-γ than F1-loaded microspheres group; which may result from F1-Al(OH)3 induced exogenous soluble antigens humoral immune response, or Th2 pathway. F1-loaded microspheres presented in the IL-4 and IFN-γ level, which may result from exogenous soluble antigen via phagocytosis induced Th1, and Th2 pathway reactions. F1-Al(OH)3 and F1-loaded microspheres group detected TNF-α expression, which may be associated with the activation of antigen-presenting cells. These results suggest that both F1 antigen-containing vaccines stimulated specific IFN-γ, TNF-α, and IL-4-type cytokines.
Only a few adjuvants are licensed for human use,14,44 Alum, the most commonly used, is a trivalent aluminum salt. It was first tested as an adjuvant in a tetanus toxin vaccine in 1926. Injection of alum causes macrophage and leukocyte migration to the injection site. Proposed mechanisms of action include entrapment/adsorption of antigens within mineral deposits for either sustained antigen release (depot effect) or enhanced antigen uptake by APCs.15,26 Alum is engulfed by macrophages, and is reported to persist inside the cell for several months. The depot effect of alum has been argued against based on continued adjuvant effects following excision of the injection site. Particulates and crystals stimulate the immune system to induce inflammatory responses. Conversely, nanometer- to micrometer-sized crystal, sphere, and hydrogel forms of aluminum salts have been used as vaccine adjuvants to enhance antibody responses in animals and humans.42,44
Parent et al45 suggest that a plague vaccine capable of inducing cell-mediated and humoral immunity would be effective against pneumonic plague. Antigen encapsulated into PLGA microspheres is good for oral administration because the polymer decreases the antigen degradation at the acid condition; also, oral delivery may result in high IgA levels. Shen et al46 and Schliehe et al47 reported that soluble antigen, or PLGA particles with surface-attached or PLGA particle encapsulated antigen, resulted in antigen uptake and CD8+ T-cell activation in dendritic cells, which increased cellular uptake of antigen and induced T-cell responses at 1,000-fold lower antigen concentration. Kuo-Haller et al16 reported that using ovalbumin delivered orally or intranasally via polymer particles to mice was effective. Repeated prime/boost at a single site results in high ovalbumin-specific antibody levels in the serum for mice immunized orally (IgA) and intravaginally (IgA and IgG) after 3 months. Nayak et al48 demonstrated that rotavirus (RV) loaded in PLA and PLGA polymer particles (size ranges between 1 and 8 μm) were evaluated in mice by oral, intranasal, and intramuscular routes of administration. They reported that between pre- and postimmunized sera, immunoglobulin A (IgA) and immunoglobulin G (IgG) titer rose ≥4-fold. PLGA encapsulated RV microparticles elicited better antibody response through the intranasal route (90%), and when administrated through oral route, PLA encapsulated RV microparticles showed 83.3% improved response.
These results clearly illustrate that intraperitoneal immunization with the Y. pestis F1-loaded PLGA/PEG microspheres could protect mice from a live Y. pestis challenge. The Y. pestis F1 antigen incorporation, physicochemical characterization data, and animal results obtained in this study may be relevant in optimizing the vaccine incorporation and delivery properties of these potential vaccine targeting carriers. In designing a vaccine, besides safety and immunogenicity, several factors were also considered, such as ease of administration and production cost. The microsphere-based retained antigen Y. pestis F1 antigen vaccine, although equipped with no untoward reactions, has a high survival rate and delivery simplicity. These factors would contribute to a low cost of the vaccination, which is suitable for developing countries where Y. pestis infection epidemics and endemics are problems of public health concern.
Conclusion
In conclusion, the Y. pestis F1 antigen-loaded PLGA/PEG microspheres using the w/o/w emulsion solvent evaporation technique was prepared successfully. Study results show that microspheres resulted in a controlled release of Y. pestis F1 antigen over 70 days. To evaluate the potential of Y. pestis F1 vaccine against Y. pestis infection, we characterize the protective efficacy and immune responses of mice subcutaneously injected with Y. pestis F1-loaded PLGA/PEG microspheres exhibited a marked decrease of morbidity, and a significant enhancement of survival. Also, a dramatic increase of F1-specific antibody titer from immunized mice measured by ELISA was noted. Physicochemical characterization data and the release result of the Y. pestis F1-loaded PLGA/PEG microspheres obtained in this study may be relevant in optimizing the incorporation of PLGA/PEG microspheres formulation into vaccine delivery in the near future.
Acknowledgments
We thank the National Science Council for a grant (NSC 98-2320-B-016-003-MY3), and the Department of Defense (DOD-98-11-07) for their partial financial support of this study.
Disclosure
The authors declare no conflicts of interest in this work.
References
Butler T. Plague gives surprises in the first decade of the 21st century in the United States and worldwide. Am J Trop Med Hyg. 2013;89(4):788–793. | |
Meyer KF. Effectiveness of live or killed plague vaccines in man. Bull World Health Organ. 1970;42(5):653–666. | |
Tiball RW, Williamson ED. Yersinia pestis (plague) vaccines. Expert Opin Biol Ther. 2004;4(6):965–973. | |
Feodorova VA, Motin VL. Plague vaccines: current developments and future perspectives. Emerg Microbes Infect. 2012;1(11):e36. | |
Wang X, Zhang X, Zhou D, Yang R. Live-attenuated Yersinia pestis vaccines. Expert Rev Vaccines. 2013;12(6):677–686. | |
Ali R, Naqvi RA, Kumar S, Bhat AA, Rao DN. Multiple antigen peptide containing B and T cell epitopes of F1 antigen of Yersinia pestis showed enhanced Th1 immune response in murine model. Scand J Immunol. 2013;77(5):361–371. | |
Thomas RJ, Webber D, Collinge A, et al. Different pathologies but equal levels of responsiveness to the recombinant F1 and V antigen vaccine and ciprofloxacin in a murine model of plague caused by small- and large-particle aerosols. Infect Immun. 2009;77(4):1315–1323. | |
Sabhnani L, Manocha M, Sridevi K, Shashikiran D, Rayanade R, Rao DN. Developing subunit immunogens using B and T cell epitopes and their constructs derived from the F1 antigen of Yersinia pestis using novel delivery vehicles. FEMS Immunol Med Microbiol. 2003;38(3):215–229. | |
Williamson ED, Oyston PC. Protecting against plague: towards a next-generation vaccine. Clin Exp Immunol. 2013;172(1):1–8. | |
Zav’yalov V, Denesyuk A, Zav’yalova G, Korpela T. Molecular modeling of the steric structure of the envelope F1 antigen of Yersinia pestis. Immunol Lett. 1995;45(1–2):19–22. | |
Zavialov AV, Berglund J, Pudney AF, et al. Structure and biogenesis of the capsular F1 antigen from Yersinia pestis: preserved folding energy drives fiber formation. Cell. 2003;113(5):587–596. | |
Powell BS, Andrews GP, Enama JT, et al. Design and testing for a nontagged F1-V fusion protein as vaccine antigen against bubonic and pneumonic plague. Biotechnol Prog. 2005;21(5):1490–1510. | |
Eldridge JH, Staas JK, Meulbroek JA, McGhee JR, Tice TR, Gilley RM. Biodegradable microspheres as a vaccine delivery system. Mol Immunol. 1991;28(3):287–294. | |
Korsholm KS. One does not fit all: new adjuvants are needed and vaccine formulation is critical. Expert Rev Vaccines. 2011;10(1):45–48. | |
Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf B Biointerfaces. 2010;75(1):1–18. | |
Kuo-Haller P, Cu Y, Blum J, Appleton JA, Saltzman WM. Vaccine delivery by polymeric vehicles in the mouse reproductive tract induces sustained local and systemic immunity. Mol Pharm. 2010;7(5):1585–1595. | |
Yeh MK, Coombes AG, Chen JL, Chiang CH. Japanese encephalitis virus vaccine formulations using PLA lamellar and PLG microparticles. J Microencapsul. 2002;19(5):671–682. | |
Wischke C, Schwendeman SP. Principles of encapsulating hydrophobic drugs in PLA/PLGA microparticles. Int J Pharm. 2008;364(2):298–327. | |
Yeht MK, Chen JL, Chiang CH. Vibrio cholerae-loaded poly(DL lactide co-glycolide) microparticles. J Microencapsul. 2002;19(2):203–212. | |
Yeh MK, Davis SS, Coombes AG. Improving protein delivery from microparticles using blends of poly(DL lactide co-glycolide) and poly(ethylene oxide)-poly(propylene oxide) copolymers. Pharm Res. 1996;13(11):1693–1698. | |
Mundargi RC, Babu VR, Rangaswamy V, Patel P, Aminabhavi TM. Nano/micro technologies for delivering macromolecular therapeutics using poly(D,L-lactide-co-glycolide) and its derivatives. J Control Release. 2008;125(3):193–209. | |
Rao DA, Forrest ML, Alani AW, Kwon GS, Robinson JR. Biodegradable PLGA based nanoparticles for sustained regional lymphatic drug delivery. J Pharm Sci. 2010;99(4):2018–2031. | |
Elkharraz K, Ahmed AR, Dashevsky A, Bodmeier R. Encapsulation of water-soluble drugs by an o/o/o-solvent extraction microencapsulation method. Int J Pharm. 2011;409(1–2):89–95. | |
Chen JL, Yeh MK, Chiang CH. The mechanism of surface-indented protein-loaded PLGA microparticle formation: the effects of salt (NaCl) on the solidification process. J Microencapsul. 2004;21(8):877–888. | |
Fredenberg S, Wahlgren M, Reslow M, Axelsson A. The mechanisms of drug release in poly(lactic-co-glycolic acid)-based drug delivery systems – a review. Int J Pharm. 2011;415(1–2):34–52. | |
Freitas S, Merkle HP, Gander B. Microencapsulation by solvent extraction/evaporation: reviewing the state of the art of microsphere preparation process technology. J Control Release. 2005;102(2):313–332. | |
Heegaard PM, Dedieu L, Johnson N, et al. Adjuvants and delivery systems in veterinary vaccinology: current state and future developments. Arch Virol. 2011;156(2):183–202. | |
Yeh M, Chiang C. Inactive Vibrio cholerae whole-cell vaccine-loaded biodegradable microparticles: in vitro release and oral vaccination. J Microencapsul. 2004;21(1):91–106. | |
Coombes AG, Yeh MK, Lavelle EC, Davis SS. The control of protein release from poly(DL-lactide co-glycolide) microparticles by variation of the external aqueous phase surfactant in the water-in oil-in water method. J Control Release. 1998;52(3):311–320. | |
Huang SS, Li IH, Hong PD, Yeh MK. Evaluation of protective efficacy using a nonstructural protein NS1 in DNA vaccine-loaded microspheres against dengue 2 virus. Int J Nanomedicine. 2013;8:3161–3169. | |
Wang Y, Hao J, Li Y, et al. Poly(caprolactone)-modified Pluronic P105 micelles for reversal of paclitaxcel-resistance in SKOV-3 tumors. Biomaterials. 2012;33(18):4741–4751. | |
Wu SF, Liao CL, Lin YL, et al. Evaluation of protective efficacy and immune mechanisms of using a non-structural protein NS1 in DNA vaccine against dengue 2 virus in mice. Vaccine. 2003;21(25–26):3919–3929. | |
Yamanaka H, Hoyt T, Yang X, et al. A nasal interleukin-12 DNA vaccine coexpressing Yersinia pestis F1-V fusion protein confers protection against pneumonic plague. Infect Immun. 2008;76(10):4564–4573. | |
Reddin KM, Easterbrook TJ, Eley SM, et al. Comparison of the immunological and protective responses elicited by microencapsulated formulations of the F1 antigen from Yersinia pestis. Vaccine. 1998;16(8):761–767. | |
Florence AT, Hillery AM, Hussain N, Jani PU. Factors affecting the oral uptake and translocation of polystyrene nanoparticles: histological and analytical evidence. J Drug Target. 1995;3(1):65–70. | |
Oyewumi MO, Kumar A, Cui Z. Nano-microparticles as immune adjuvants: correlating particle sizes and the resultant immune responses. Expert Rev Vaccines. 2010;9(9):1095–1107. | |
Rosli R, Nograles N, Hanafi A, Nor Shamsudin M, Abdullah S. Mucosal genetic immunization through microsphere-based oral carriers. Hum Vaccin Immunother. 2013;9(10). | |
Thomas C, Gupta V, Ahsan F. Influence of surface charge of PLGA particles of recombinant hepatitis B surface antigen in enhancing systemic and mucosal immune responses. Int J Pharm. 2009;379(1):41–50. | |
He J, Feng M, Zhou X, et al. Stabilization and encapsulation of recombinant human erythropoietin into PLGA microspheres using human serum albumin as a stabilizer. Int J Pharm. 2011;416(1):69–76. | |
Heo S, Lee M, Lee S, Sah H. Investigation on structural integrity of PLGA during ammonolysis-based microencapsulation process. Int J Pharm. 2011;419(1–2):60–70. | |
Li M, Rouaud O, Poncelet D. Microencapsulation by solvent evaporation: state of the art for process engineering approaches. Int J Pharm. 2008;363(1–2):26–39. | |
Li Z, Zhang L, Sun W, Ding Q, Hou Y, Xu Y. Archaeosomes with encapsulated antigens for oral vaccine delivery. Vaccine. 2011;29(32):5260–5266. | |
Mata E, Igartua M, Patarroyo ME, Pedraz JL, Hernández RM. Enhancing immunogenicity to PLGA microparticulate systems by incorporation of alginate and RGD-modified alginate. Eur J Pharm Sci. 2011;44(1–2):32–40. | |
Kuroda E, Coban C, Ishii KJ. Particulate adjuvant and innate immunity: past achievements, present findings, and future prospects. Int Rev Immunol. 2013;32(2):209–220. | |
Parent MA, Berggren KN, Kummer LW, et al. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect Immun. 2005;73(11):7304–7310. | |
Shen H, Ackerman AL, Cody V, et al. Enhanced and prolonged cross-presentation following endosomal escape of exogenous antigens encapsulated in biodegradable nanoparticles. Immunology. 2006;117(1):78–88. | |
Schliehe C, Redaelli C, Engelhardt S, et al. CD8- dendritic cells and macrophages cross-present poly(D,L-lactate-co-glycolate) acid microsphere-encapsulated antigen in vivo. J Immunol. 2011;187(5):2112–2121. | |
Nayak B, Ray AR, Panda AK, Ray P. Improved immunogenicity of biodegradable polymer particles entrapped rotavirus vaccine. J Biomater Appl. 2011;25(5):469–496. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




