Back to Journals » Therapeutics and Clinical Risk Management » Volume 10
Determinants of decision-to-intervention time in the management and therapeutic outcome of emergency gynecological surgeries in south east Nigeria
Authors Onyebuchi A, Lawani L, Nkwo PO, Iyoke CA , Onoh R, Ajah L
Received 28 April 2014
Accepted for publication 22 May 2014
Published 28 July 2014 Volume 2014:10 Pages 577—582
DOI https://doi.org/10.2147/TCRM.S66897
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Azubuike Kanario Onyebuchi,1 Lucky Osaheni Lawani,2 Peter O Nkwo,3 Chukwuemeka Anthony Iyoke,3 Robinson Chukwudi Onoh,1 Leonard O Ajah1
1Department of Obstetrics and Gynecology, Federal Teaching Hospital Abakaliki, Ebonyi State, Nigeria; 2School of Postgraduate Studies, Department of Community Medicine, University of Nigeria, 3Department of Obstetrics and Gynecology, University of Nigeria Teaching Hospital, Enugu, Enugu State, Nigeria
Background: Prompt and timely response in the management of gynecological surgical cases can significantly affect the therapeutic surgical outcome of patients in emergency situations. The aim of this study was to evaluate the decision-to-intervention time (DIT), its determinants, and the significance in the therapeutic outcome of emergency gynecological surgeries managed at a federal teaching hospital in south east Nigeria over an 18-month period.
Methods: This was a prospective descriptive study of 105 emergency gynecological cases managed at a federal teaching hospital over an 18-month period. Patients were recruited at the point of admission and followed up until discharge for outcome. Data were abstracted with a data entry pro forma and then analyzed with the Epi Info™ statistical software version 7.0.
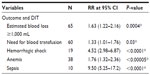
Results: The incidence of gynecological surgical emergencies was 5.1% of the total gynecological cases managed during the study period. The mean DIT was 4.25 (range 1.45–5.50) hours with delay in intervention, mainly due to delays in securing blood/blood products and other materials for resuscitation (46.7%) and a lack of finance (15.2%). Six maternal deaths were recorded, giving a case fatality ratio of 5.7%, while the commonest maternal complications associated with the delays were hemorrhage (61.9%) and the need for blood transfusion (57.1%), respectively. The risk ratio of losing ≥1,000 mL of blood, anemia, hemorrhagic shock, and wound infection in those with DIT ≥120 minutes was statistically greater and significant at 95% confidence interval.
Conclusion: Inadequacies in health care services and policies due to poor infrastructure, organizational framework, and financing were the major determinants of the prolonged DIT and therapeutic outcomes.
Keywords: determinants, decision-to-intervention time, emergency, therapeutic outcome, gynecological surgeries, clinical risk
Background
Gynecological emergencies constitute a significant proportion of the workload of most gynecologists, and in many low- and middle-income countries, the management of gynecological emergencies presents enormous challenges, especially in managing clinical risk, given the weak infrastructure and the health care system.1,2 Delays in decision making and instituting interventions could result in rapid decompensation, serious morbidity, or loss of life. Prompt response is the key to clinical risk management and the survival of patients.2 It may be rational to anticipate that the determinants of prolonged decision-to-intervention time (DIT) in emergency gynecological surgeries may not be too different from those identified in obstetrics practice.3–5 However, the factors especially in low-income settings are often multiple and complex and may include: a huge load of severe cases; nonavailability of hospital consumables and materials for resuscitation and definitive treatment at critical times; logistics of transferring patients to operating theaters; poor response time; inadequacy and/or lack of facilities and personnel; delay in administration of anesthesia; and the absence of any clear policy toward ensuring prompt and adequate treatment for life-threatening emergencies.5–7
Considering that women could suffer severe morbidity and mortality from delays in the time from DIT in emergency situations and the fact that there are limited local and international data on the topic, this study was designed to evaluate: the determinants; therapeutic outcomes and significance of DIT in resuscitation; and the offer of definitive treatment in situations of gynecologic surgical emergencies.
Materials and methods
This was a prospective descriptive study of all 105 cases of emergency gynecological surgeries managed from January 1, 2012–June 30, 2013, at the government-owned (public) Federal Teaching Hospital in Abakaliki, Ebonyi State, in south east Nigeria. Based on the 2006 national population census, the state has a population of 2,176,947 (1,064,156 males and 1,112,791 females).8 The population of the state is predominantly rural. The facility provides specialized gynecological services to women in the state, and it also receives referrals from the other neighboring south east Nigerian states. The fees for service/user charges for the treatment received in this health facility were borne by the clients. Ethical clearance was obtained from the research ethics committee of the hospital. Written and signed consents for treatment and participation in the study were obtained from the participants themselves or from their next of kin in moribund cases. The 105 cases of emergency gynecological surgeries met the criteria for gynecologic emergencies, which we defined to include all acute or complicated life-threatening gynecological cases that required immediate therapeutic interventions; they all consented to treatment and participation in the study.
During the study period, 2,067 gynecological cases were managed in the facility. A standard data entry pro forma was used to collect data on sociodemographic characteristics, diagnosis, type of surgical interventions and indication, DIT and its determinants, clinical risk associated with the delays in the therapeutic interventions, and immediate therapeutic outcomes.
The data were abstracted by resident doctors in the emergency department, theater, and gynecological wards of the hospital’s Department of Obstetrics and Gynecology. The DIT was defined as the time interval between when the decision to undertake surgery was made to the time the incision on the skin was made. Hemorrhage was defined as an estimated blood loss of ≥1,000 mL or any blood loss significant enough to compromise the hemodynamic status of the patient. DIT was evaluated by assigning to a member of each managing team the responsibility of noting and documenting the time from when a decision to surgically intervene was taken to the time surgical incision on the skin was made for each case.
The data were analyzed with Epi Info™ statistical software version 7.0 (Centers for Disease Control and Prevention, Atlanta, GA, USA). The process involved the calculation of mean, median, range, percentages, and inferential statistics to determine the risk ratio at 95% confidence interval, test of statistical significance was by Fisher’s exact test (probability two-tailed) and Pearson’s chi-squared test; P-value <0.05 was considered statistically significant.
Results
The incidence of gynecological surgical emergencies was 5.1% of the total gynecological cases managed during the study period. Table 1 represents the sociodemographic characteristics of the participants with the majority (69.5%) living in rural areas, while Table 2 shows the various indications for emergency exploratory laparotomy and definitive therapeutic surgery – with ruptured ectopic pregnancy being the commonest indication (59.0%). None of the cases had therapeutic surgical intervention within 30 minutes of the decision to do so. The mean DIT in the study center was 4.25 (range 1.45–5.50) hours, while the median was 3.92 hours. Delays in DIT were attributed to the reasons stated in Table 3, which included: nonavailability of blood/blood products/other resuscitation materials (46.7%); inability to afford the cost of treatment (15.2%); nonavailability of medications and surgical materials (11.4%); delays in obtaining preoperative laboratory results (11.4%); delay in transferring patient and lack of operating theater space (5.7%); delays in the administration of anesthesia (3.8%); unavailability and inadequacy of health care providers (2.9%); and equipment failure (1.0%).
  | Table 2 Emergency gynecological surgeries and their indications, N=105* |
  | Table 3 Major reasons for delay >60 minutes from DIT* |
Table 4 shows the clinical outcome of emergency gynecological surgeries; blood loss .1,000 mL was a significant morbidity, which necessitated blood transfusion (57.1%) for hemorrhagic shock (18.1%) and anemia (36.2%). Six deaths were recorded, giving a case fatality rate of 5.7%. The mean DIT for the deaths recorded was 4.51±0.68 hours. The deaths recorded were in those who had a perforated uterus and pelvic abscess. The deaths were due to sepsis (66.7%), hemorrhage (33.3%) complicated by disseminated intravascular coagulopathy, and renal failure before surgical intervention despite the decision to do so.
  | Table 4 Therapeutic outcome of emergency gynecological surgeries* |
Table 5 depicts the comparison of the therapeutic outcome of the surgery based on a DIT of ≤120 minutes and >120 minutes. The risk ratio of losing ≥1,000 mL of blood, anemia, hemorrhagic shock, need for blood transfusion, and sepsis in those with DIT ≥120 minutes was statistically greater and significant at 95% confidence interval.
Discussion
The management of gynecological emergency is directed at the preservation of life, health, sexual function, and fertility by minimizing or elimination of clinical risk via quick therapeutic interventions.9 Surgical emergencies may periodically occur at any time in any setting. In responding to such emergencies, it is important that gynecologists prepare themselves to assess and intervene without undue delay to prevent life threatening clinical risk in the form of morbidity and mortality.10
Prolonged delays in providing the needed interventions in the situations of gynecological surgical emergencies can adversely affect the therapeutic outcome of the patient,9 most especially in low resource settings where late referrals for specialized care commonly occurs only when patients are already in a moribund state.5,11,12
The 5.1% incidence of gynecological surgical emergencies in this study is a reflection that gynecological emergencies constitute a significant proportion of gynecological cases seen in the study center during the period under review and need to be given proper attention to avert worsening of the already dismal health indices in this setting. This incidence is however less than the 9.6% reported in Kasur, Pakistan;11 however, no local data were available to make a comparison.
Emergency exploratory laparotomy for ruptured ectopic pregnancy is arguably considered one of the most common gynecological emergency surgeries performed in contemporary gynecological practice.1,2 It was, therefore, not surprising that it constituted 59% of the total gynecological surgical emergencies managed during the study period. This is similar to the findings of other researchers, where it accounted for 61% of gynecological emergencies in India, but was, however, less than the 6.5% reported in Kebbi in northern Nigeria.2,9 Ruptured ectopic pregnancy has been associated with severe morbidity and mortality.2,10,13 The morbidity and mortality have also been associated with the delays in instituting prompt resuscitative measures and treatment interventions.13
Adnexal torsion in the form of torsion of an ovarian cyst is one of the gynecologic surgical emergencies reported in this and similar studies. It has been associated with permanent sequelae, including the loss of an ovary with an impact on future fertility, peritonitis, and even death if there are delays in surgical intervention.14 The other indication for emergency exploratory laparotomy in this study is similar to those reported by other researchers.2,9,11
It has been reported that – without quick interventions – the indications for emergency gynecological surgeries (Table 2) may endanger the life of women and significantly affect their treatment outcome.2,9,10 This emphasizes the need to have a practice guideline or protocol that encourages quick treatment interventions in gynecological emergencies. This should be part of various local, national or international guidelines, and recommendations to minimize the risks of adverse outcome. The mean DIT for emergency gynecological surgeries in this study was 4.25 (range 1.45–5.50) hours; comparison of this mean value with findings elsewhere was difficult because of the general absence of data on the topic. However, even though no standard or ideal DIT in gynecology has been universally agreed and accepted as appropriate, there are reports in obstetrics practice that prolonged DIT well above 75 minutes in one study and 3 hours in another study were associated with greater adverse maternal and perinatal outcomes.15–18
The identified causes of delay in DIT for surgical emergencies – such as the nonavailability of blood/blood products, delay in administration of anesthesia, nonavailability/inadequacy of care providers, transfer of patient to theater, lack of theater space, getting preoperative laboratory results, obtaining consent for surgery from patients/next of kin who often decline, the patient’s lack of finance – are all not particularly peculiar but rather similar to those reported in other countries and similar settings.5–7,18–19
Research has shown that these determinants of the prolonged DIT identified in this study and similar studies are preventable and can be averted or improved upon, using evidence-based interventions or models that address such delays.20,21 In view of these findings, the implications, and the significance on treatment outcome, there is a need to institute interventions aimed at reducing the DIT in health facilities and addressing the delayed referral of complicated cases in our effort to reduce the DIT for emergency cases to ensure improvement, since prolonged DIT has been associated with poor treatment outcome in both low-, middle-, and even high-income countries.2,3,5,10
To address the determinants or identified causes of delays, increasing the women’s awareness and those of their next of kin that surgical intervention (that would require consent) might be required could reduce the waiting time before surgery. To ensure prompt response in emergency situations, caregivers (health personnel) should be available at all times and provided with efficient communication and transport arrangement to address situations where experienced health personnel are not in-house at critical times as shown in this and other studies.15 It was noted in an audit by Tuffnell et al that 12 of 29 delays of >50 minutes were due to multiple attempts at spinal anesthesia.17 Thus, delays in the administration of anesthesia – especially regional anesthesia like spinal and epidural – should be avoided.
There is need to establish a quality improvement team in every unit. The goal of this team should be to decrease the DIT for all emergency gynecological surgical emergencies to an interval that will be safe for women. This can be achieved through a well-coordinated multidisciplinary team approach that includes nurses, gynecologist, anesthetist, laboratory scientist, and other members of the health team. The team should have regular drills as part of the training and retraining process to ensure early and prompt interventions by the experienced and inexperienced.
There is a need for the health care service administrators to ensure that more than one emergency operating theater is available and accessible within a few minutes of the decision to operate. They should also ensure the availability of complete surgical packs/kits and medical consumables to be ready at all times for emergency cases, since this lack has been identified as a major cause of delay. Because hemorrhage is a leading cause of morbidity and mortality in this environment,22 establishing a functional, efficient, and responsive blood bank system to provide blood/blood products for the transfusion – which may be needed as part of the materials for resuscitation and surgery in bleeding cases – is necessary. To also reduce the DIT for emergency surgeries, an efficient laboratory system or unit (one that is strictly dedicated to the maternity and gynecology unit to ensure laboratory results) is expected to be made available within the shortest possible time frame.
A national health insurance scheme and policy with optimal financing that will care for all – despite their social status – will go a long way to address the issue of lack of finance. There should be regular audits to address challenges and to ensure that sustainable progress has been made.
Strength and limitation of study
The major strength of this present study is its prospective nature, which made the process of data collection easy and complete; however, a larger, multicentered study that involved similar practice settings would give a better measure of outcome.
Conclusion
The findings from this study indicate that inadequacies in health care services due to poor infrastructure, organizational framework, and financing – as well as the absence of local protocol or practice guidelines for clinical management of high-risk emergencies – were identified as major factors that resulted in the avoidable prolongation of DIT with poor therapeutic outcomes, and that the care received by the women with gynecological surgical emergencies is still suboptimal in emergency situations, resulting in poor treatment outcomes. These are indications of the existing loopholes in our current health care policies and its implementation, and forms the basis to review and upgrade existing policies and implementation strategies.
Acknowledgments
The authors extend their gratitude to all participants in this study. They are also indebted to the staff of the emergency, theater, and gynecology departments for their excellent cooperation and support in data collection during the study period.
Author contributions
The work presented here was carried out in collaboration between all authors. All authors defined the research theme. AKO, LOL and PON designed methods and collected data, analyzed the data and interpreted the results. AKO, LOL, RCO, CAI codesigned the methods, conducted the data analysis, and coworked on the associated data collection and their interpretation. All the authors were involved in drafting the article or revising it critically for important intellectual content. All authors have approved the manuscript. All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Fawole AO, Awonuga DO. Gynaecological Emergencies in the Tropics: Recent Advances in Management. Annals of Ibadan Postgraduate Medicine. 2007;5(1):12–20. | |
Pattern and outcome of gynaecological emergencies at a Nigerian secondary Health Care Centre [webpage on the Internet]. Sugar Land, TX: The Internet Journal of Tropical Medicine; 2009 [cited January 28, 2014]. Available from: http://ispub.com/IJTM/6/2/8447. Accessed December 24, 2013. | |
American Academy of Pediatrics. Guidelines for Perinatal Care. 5th ed. Washington, DC: American Academy of Pediatrics and The American College of Obstetricians and Gynecologists; 2002. | |
American College of Obstetricians and Gynecologists. ACOG Committee Opinion no 256: Committee on Obstetric Practice. Optimal goals for anesthesia care in obstetrics. Obstet Gynecol. 2001;97(5 Pt 1): Suppl 1–3. | |
Gohou V, Ronsmans C, Kacou L, et al. Responsiveness to life-threatening obstetric emergencies in two hospitals in Abidjan, Côte d’Ivoire. Trop Med Int Health. 2004;9(3):406–415. | |
Hillemanns P, Hepp H, Rebhan H, Knitza R. [Emergency cesarean section – organization and decision-delivery time]. Geburtshilfe Frauenheilkd. 1996;56(8):423–430. German [with English abstract]. | |
Thomas J, Paranjothy S, James D. National cross sectional survey to determine whether the decision to delivery interval is critical in emergency caesarean section. BMJ. 2004;328(7441):665. | |
State population [webpage on the Internet]. Abuja: Nigeria. National Population Commission; 2006 [Cited February 20, 2014]. Available from www.population.gov.ng/index.php/state-population. Accessed July 14, 2014. | |
Pokharel HP, Dahal P, Rai R, Budhathoki SS. Surgical emergencies in obstetrics and gynaecology in a tertiary care hospital. JNMA J Nepal Med Assoc. 2013;52(189):213–216. | |
American College of Obstetricians and Gynecologists Committee on Patient Safety and Quality Improvement. ACOG Committee Opinion No 487: Preparing for clinical emergencies in obstetrics and gynecology. Obstet Gynecol. 2011;117(4):1032–1024. | |
Sardar A, Syed TAS. Gynaecological emergencies. Professional Med J. 2007;14(1):43–48. Available from http://www.pakmedinet.com/11582. Accessed July 14, 2014. | |
Roopa PS, Verma S, Rai L, Kumar P, Pai MV, Shetty J. “Near miss” obstetric events and maternal deaths in a tertiary care hospital: an audit. J Pregnancy. 2013;2013:393758. | |
Lawani OL, Anozie OB, Ezeonu PO. Ectopic pregnancy: a life-threatening gynecological emergency. Int J Womens Health. 2013;5:515–521. | |
Sasaki KJ, Miller CE. Adnexal torsion: review of the literature. J Minim Invasive Gynecol. 2014;21(2):196–202. | |
Nasrallah FK, Harirah HM, Vadhera R, Jain V, Franklin LT, Hankins GD. The 30-minute decision-to-incision interval for emergency cesarean delivery: fact or fiction? Am J Perinatol. 2004;21(2):63–68. | |
MacKenzie IZ, Cooke I. What is a reasonable time from decision-to-delivery by caesarean section? Evidence from 415 deliveries. BJOG. 2002;109(5):498–504. | |
Tuffnell DJ, Wilkinson K, Beresford N. Interval between decision and delivery by caesarean section-are current standards achievable? Observational case series. BMJ. 2001;322(7298):1330–1333. | |
Helmy WH, Jolaoso AS, Ifaturoti OO, Afify SA, Jones MH. The decision-to-delivery interval for emergency caesarean section: is 30 minutes a realistic target? BJOG. 2002;109(5):505–508. | |
Onah HE, Ibeziako N, Umezulike AC, Effetie ER, Ogbuokiri CM. Decision – delivery interval and perinatal outcome in emergency caesarean sections. J Obstet Gynaecol. 2005;25(4):342–346. | |
Mooney SE, Ogrinc G, Steadman W. Improving emergency caesarean delivery response times at a rural community hospital. Qual Saf Health Care. 2007;16(1):60–66. | |
Sayegh I, Dupuis O, Clement HJ, Rudigoz RC. Evaluating the decision-to-delivery interval in emergency caesarean sections. Eur J Obstet Gynecol Reprod Biol. 2004;116(1):28–33. | |
Lawani OL, Iyoke CA, Onyebuchi AK. Blood transfusion trends in obstetrics at the Federal Teaching Hospital in Abakaliki, South-East Nigeria. Int J Womens Health. 2013;5:407–412. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.