Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Defensive function of persecutory delusion and discrepancy between explicit and implicit self-esteem in schizophrenia: study using the Brief Implicit Association Test
Authors Nakamura M, Hayakawa T, Okamura A, Kohigashi M, Fukui K, Narumoto J
Received 7 September 2014
Accepted for publication 20 October 2014
Published 22 December 2014 Volume 2015:11 Pages 33—40
DOI https://doi.org/10.2147/NDT.S73906
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Roger Pinder
Mitsuo Nakamura,1 Tomomi Hayakawa,2 Aiko Okamura,3 Mutsumi Kohigashi,4 Kenji Fukui,1 Jin Narumoto1
1Department of Psychiatry, Graduate School of Medicine, Kyoto Prefectural University of Medicine, Kyoto, Japan; 2Gojouyama Hospital, Nara, Japan; 3Yashio Hospital, Saitama, Japan; 4Department of Psychiatry, Kyoto Second Red Cross Hospital, Kyoto, Japan
Background: If delusions serve as a defense mechanism in schizophrenia patients with paranoia, then they should show normal or high explicit self-esteem and low implicit self-esteem. However, the results of previous studies are inconsistent. One possible explanation for this inconsistency is that there are two types of paranoia, “bad me” (self-blaming) paranoia and “poor me” (non-self-blaming) paranoia. We thus examined implicit and explicit self-esteem and self-blaming tendency in patients with schizophrenia and schizoaffective disorder. We hypothesized that patients with paranoia would show lower implicit self-esteem and only those with non-self-blaming paranoia would experience a discrepancy between explicit and implicit self-esteem.
Methods: Participants consisted of patients with schizophrenia and schizoaffective disorder recruited from a day hospital (N=71). Participants were assessed for psychotic symptoms, using the Brief Psychiatric Rating Scale (BPRS), and self-blaming tendency, using the brief COPE. We also assessed explicit self-esteem, using the Rosenberg Self-Esteem Scale (RSES), implicit self-esteem, using Brief Implicit Association Test (BIAT), and discrepancy between explicit and implicit self-esteem.
Results: Contrary to our hypothesis, implicit self-esteem in paranoia and nonparanoia showed no statistical difference. As expected, only patients with non-self-blaming paranoia experienced a discrepancy between explicit and implicit self-esteem; other groups showed no such discrepancy.
Conclusion: These results suggest that persecutory delusion plays a defensive role in non-self-blaming paranoia.
Keyword: coping style, poor me paranoia, remitted paranoid delusion, external attribution
Introduction
A number of theories have been provided to explain the mechanism of persecutory delusion. Self-esteem has been hypothesized to play an important role, but the relationship between paranoia and self-esteem is controversial.1 Garety and Freeman argued that persecutory delusion is a direct reflection of negative emotion.2 However, Bentall et al proposed that paranoid thought is a defense against negative affection.3 According to this view, persecutory delusion is a product of attributional processes to maintain a positive self-esteem against negative events. Patients with paranoia are thus considered to have implicit low self-esteem; however, persecutory delusion serves to mask their covert low self-esteem by attributing the source of threats to external causes.
If delusion had a defensive function, then patients with persecutory delusion should show normal or higher explicit self-esteem and lower implicit self-esteem.4 Explicit self-esteem is usually assessed using questionnaires. Implicit self-esteem is defined as an automatic and hidden attitude toward the self, and there are many other examples of dissociation between automatic reactions and more deliberative ones. However, research on this topic has not yielded consistent results. Some studies have shown that patients with persecutory delusions have high self-esteem,5,6 while others found it associated with low self-esteem.7 Moreover, the few studies on implicit self-esteem have found inconclusive results.6,8–14
Differences between previous findings may result from reliability of implicit self-esteem. The implicit association test (IAT) is a method that assesses the strength of associations between concepts and is the most appropriate measure of implicit self-esteem;15 however, it was not used in some studies.6,8,11
The inconsistent results also may be due to different types of paranoia: “bad me” and “poor me”.16 In “bad me” paranoia, the self is experienced as bad and deserves blaming, leading to low self-esteem. “Bad me” paranoia is manifested by constant struggle to avoid criticism by others through an avoidant attachment style. Conversely, people with “poor me” paranoia perceive themselves as good and reject others’ malevolence as undeserved persecution, resulting in relatively higher self-esteem compared with “bad me” patients.16 The discrepancy between explicit and implicit self-esteem is hypothesized to exist in only “poor me” patients. However, there has so far been no comparison of explicit and implicit self-esteem in “poor me” and “bad me” paranoia groups.
Another possible explanation for the contradictory results is that the defensive function of delusion may be seen in only remitted paranoia. In remitted paranoia, although antipsychotic medications have reduced the symptoms exhibited, the patient has not yet reached full remission. The patient is still deluded, however less preoccupied with the delusion. Psychological processes are thought to play an important role in the maintenance of delusions and in preventing the falsification of delusional ideas in remitted paranoia.17
Our primary hypothesis was that persecutory delusion serves as a defensive function to maintain self-esteem through avoidance of negatively evaluated mental experiences. The present study tested two hypotheses: first, that patients with persecutory delusion will show lower implicit self-esteem than nonparanoid patients, regardless of whether their explicit self-esteem is high or low; and second, that the discrepancy between explicit and implicit self-esteem is predominant in only patients with paranoia who attempt to avoid blaming themselves and that patients with paranoia who tend to engage in self-blame will show no such discrepancy. We did not expect to find this pattern of results in patients who do not currently display paranoid symptoms.
Methods
Participants
Participants were recruited from the day care unit in Gojouyama hospital, and consisted of patients diagnosed with schizophrenia or schizoaffective disorder according to International Classification of Diseases (ICD)-tenth revision.18 To limit the sample to patients with remitted paranoia, those who were admitted in the previous 6 months were excluded. Patients with substance abuse, organic brain disorder, or mental retardation were also excluded.
The study was approved by the ethics committee of Gojouyama hospital. All participants provided written informed consent. The assessment of participants was conducted by three experienced psychiatrists.
Measures
Psychiatric symptoms
Brief Psychiatric Rating Scale (BPRS)
The Brief Psychiatric Rating Scale (BPRS)19 was used to evaluate the severity of psychiatric symptoms. Each of the 18 BPRS items is scored on a seven-point scale (0 to 6), with higher scores indicating more severe symptoms. 3 points indicates mild symptoms. Item 11 (suspiciousness/paranoid ideas) served as an index for delusions of persecution (BPRS Item 11 [3 points indicates mild symptoms]). Positive and negative symptoms are represented by the total scores from five items (ranging from 0 to maximum 30) and three items (ranging from 0 to maximum 18), respectively.20 The total BPRS score is the sum of scores for all items (ranging from 0 to maximum 108).
Paranoia Checklist (PCL)
To assess paranoid thought, the Japanese version of the PCL21 was used.22 The checklist consists of 18 self-report items, each rated on a five-point scale (ranging from 1= “not at all applicable” to 5= “extremely applicable”, with a possible score ranging from 18 to 90), that evaluate the frequency, degree of conviction, and level of distress experienced. The checklist has good internal reliability and is considered appropriate to measure subclinical persecutory ideation.22
Montgomery Åsberg Depression Rating Scale (MÅDRS)
The MÅDRS23 has been established as a reliable measure of severity of current depression. It is composed of ten items rated on a seven-point scale (0 to 6) and assesses factors such as sadness, tension, reduced sleep, reduced appetite, and difficulty in concentration. Scores from each item are totaled, with higher scores indicating more severe depression (ranging from 0 to maximum 60).
Coping style
Brief COPE
The brief COPE,24 a 28-item instrument, was used to assess how often respondents use 14 types of coping strategies (behavioral disengagement, denial, seeking emotional support, positive reframing, humor, acceptance, religion, venting, self-blame, self-distraction, substance use, active coping, seeking instrumental support, and planning), assessed with two items for each strategy. Items are rated on a four-point scale ranging from 0= “not at all” to 3= “a lot”. Participants were instructed to rate their coping skills in response to stressful events in general, rather than focus on how they cope with the symptoms.
Explicit self-esteem
Rosenberg Self-Esteem Scale (RSES)
The RSES25,26 is a self-report measure of global self-esteem. The scale comprises ten items, of which five are worded positively and five negatively. The items are answered on a four-point scale ranging from 1= “strongly disagree” to 4= “strongly agree”, with higher scores indicating higher self-esteem. Possible scores on RSES range from 10 to 40.
Implicit self-esteem
Brief Implicit Association Test (BIAT)
We used the BIAT27 to assess implicit self-esteem. The shorter version of the standard IAT was used due to its ease of administration on the target population.
In the BIAT, a target word appears in the center of the computer screen while categories are presented at the top of the screen. The participants are requested to classify sequences of words into superordinate categories. Superordinate categories were either “self or positive” or “other or positive”. The target words in the center of the computer screen were “self” (I, first name, surname), “other” (first name of the other person), “positive” (good, wonderful, strong, superb) and “negative” (bad, poor, weak, pity).
The participants’ task was to press a right-hand response key if the word was included in either of the two categories and a left-hand response key otherwise. Quicker response times correspond to stronger association, with small differences in speed between compatible and incompatible categories indicating low implicit self-esteem. The order of the two blocks was counterbalanced across subjects. BIAT data with more than 30% errors were omitted from the analyses.28 The D-score was calculated to compute the IAT-effect,29 with higher scores indicating a stronger association between the self and positive adjectives.
Statistical analyses
Participants were divided into groups based on paranoia (patient with scores ≥3 on item 11 on the BPRS) and self-blame (participants with scores ≥ the median score on the Brief COPE self-blame items). The four groups were classified as: self-blame paranoia (SB-P), non-self-blame paranoia (NSB-P), self-blame nonparanoia (SB-NP), and non-self-blame nonparanoia (NSB-NP).
All analyses were conducted with SPSS version 22.0 for Windows. Statistical significance was set at P<0.05 (two-tailed). Differences between sociodemographic variables, clinical data, and levels of implicit and explicit self-esteem between groups were tested using analysis of variance (ANOVA), analysis of covariance (ANCOVA), and two-tailed t-tests. To compare explicit and implicit self-esteem, all data were standardized with z-scores.11 Paired samples t-tests were conducted for each group.
Results
Demographic and clinical data
In all, 108 referrals were received, from which 94 (87%) patients agreed to participate in the study. From this group, participants with more than 30% errors in their BIAT data were excluded,28 leaving 71 participants. Seventy participants had a diagnosis of schizophrenia; one had a diagnosis of schizoaffective disorder. Figure 1 shows the selection process and classification stages of the study. Forty of the participants were male, 31 were female. Descriptive statistics of the sample are presented in Table 1. All patients were receiving antipsychotic medication at the time of assessment. The mean age was 45.4 (standard deviation [SD] =10.7) years, mean duration of illness was 20.6 (SD =11.5) years, mean chlorpromazine equivalent dose was 657.4 (SD =447.8) mg, and mean global assessment of functioning was 36.2 (SD =7.9).
  | Figure 1 The selection process and classification stages of the study. |
Of the 71 participants, 35 and 36 were assigned to the paranoia group and nonparanoia group, respectively. The median score on the Brief COPE self-blame item was 3 (range 0 to 6). Fourteen participants were classified into the NSB-P group, 21 into the SB-P group, 20 into the NSB-NP group, and 16 into the SB-NP group. Statistical analyses of group for age, sex, duration of illness, antipsychotics dosage, and global assessment of functioning revealed no significant differences between groups in terms of these factors. Grandiose delusion was found in very few participants.
A one-way ANOVA on the MÅDRS total score revealed statistically significant differences between groups (F [3, 67] =4.560, P<0.01). Participants in the NSB-NP group had less severe depression compared with those in the SB-P group. We conducted an analysis to test the homogeneity of regression and found depression was not an appropriate covariate for statistical assessment.
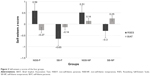
Explicit and implicit self-esteem
The results for explicit and implicit self-esteem are depicted in Table 2. The mean RSES score of the paranoia group was 24.2 (SD =5.3) and that of the nonparanoia group was 25.6 (SD =4.0), and the difference was not significant (t [69] =−1.27, P=0.21). The mean BIAT D-score of the paranoia group was 0.53 (SD =0.29) and of the nonparanoia group was 0.66 (SD =0.38). Contrary to our hypothesis, implicit self-esteem of the paranoia group showed no significant difference from the nonparanoia group. (t [69] =−1.65, P=0.10).
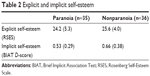  | Table 2 Explicit and implicit self-esteem |
Discrepancy between implicit and explicit self-esteem
The z-scores of each group for implicit and explicit self-esteem are shown in Figures 2 and 3. As expected, paired samples t-tests showed significant differences between explicit and implicit self-esteem in only the NSB-P group (t [20] =4.42, P=0.01), while the other groups showed no such discrepancy.
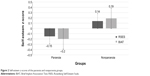  | Figure 2 Self-esteem z-scores of the paranoia and nonparanoia groups. |
The z-scores for implicit self-esteem were subtracted from the z-scores for explicit self-esteem. Positive scores indicated higher explicit than implicit self-esteem. An ANOVA of the groups for the discrepant scores revealed a significant effect of self-esteem. The NSB-P group showed significantly higher discrepancy compared with the SB-P group (P=0.03) and SB-NP group (P=0.04), but not the NSB-NP group (P=0.74).
Discussion
The present study investigated the hypothesis that persecutory delusions serve as a defense against negative self-esteem. This was the first study to classify patients with paranoid delusions according to their self-blaming tendencies and to compare explicit and implicit self-esteem for each group. Moreover, all participants of our study had remitted paranoia. As expected, the patients with remitted paranoia who avoided self-blame were able to maintain relatively high explicit self-esteem. Psychological processes are thought to play an important role in maintaining such delusions.
As expected, only participants with non-self-blame paranoia showed a discrepancy between explicit and implicit self-esteem, with higher explicit self-esteem than implicit self-esteem. Our results are consistent with the account that external attributions for negative events are found in only “poor me” patients,30 and support the hypothesis that remitted paranoid delusions have a defensive function. Our results can also account for the inconsistent results observed in previous studies, which might have been due to consideration of patients with both types of paranoia as a homogenous sample.6–13
There were some limitations in the present study, however. First, this was a cross-sectional study, and we therefore were unable to explore the causality between delusion, self-esteem, and coping style in schizophrenia. More importantly, Melo et al pointed out that “poor me” and “bad me” tendencies vary across time30 and that self-esteem is highly unstable in paranoia. We were thus also unable to explore whether our results were stable or dependent on the current clinical state. Second, a rather small sample was recruited, limiting the generalizability of the findings. Third, despite the advantages of the BIAT with regard to its properties, the BIAT should not be regarded as a pure measure of self-esteem because of its bipolar nature, ie, self vs other. The BIAT measures not only how they experience themselves, but also how they experience others. In addition, it is a relative measure, thus, it was not possible to interpret the evaluations of the self independently of the other.31 Fourth, 23 participants were excluded from analysis, which was a considerable number, considering our original sample size. Fifth, all participants of our study were in clinical remission, and they had very low BPRS scores with a narrow range. This could explain the association between paranoia and discrepancies between implicit and explicit self-esteem; however, this also could be a limitation. Finally, external attributional style is thought to play an important role in maintenance of persecutory delusion; however, we did not assess attributional style. Nevertheless, despite these limitations, our findings support the hypothesis that paranoid delusions during remission have a defensive function. Our study did not support the “delusion as expression model”.1 Being aware of such delusions could be threatening for the patients, because they fail to raise their self-esteem. Our findings are consistent with the previous study that demonstrated an association between insight and suicidal behavior.32
In summary, the present results underline the relevance of low covert self-esteem in paranoia patients; however, these results did not differ significantly from those of the nonparanoia group. Patients with paranoia who tend to avoid self-blame were found to have higher explicit than implicit self-esteem.
Disclosure
The authors report no conflicts of interest in this work.
References
Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27(4):425–457. | ||
Garety PA, Freeman D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. 1999;38(Pt 2):113–154. | ||
Bentall RP, Kinderman P, Kaney S. The self, attributional processes and abnormal beliefs: towards a model of persecutory delusions. Behav Res Ther. 1994;32(3):331–341. | ||
Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: a review and theoretical integration. Clin Psychol Rev. 2001;21(8):1143–1192. | ||
Kinderman P. Attentional bias, persecutory delusions and the self-concept. Br J Med Psychol. 1994;67(Pt 1):53–66. | ||
Lyon HM, Kaney S, Bentall RP. The defensive function of persecutory delusions. Evidence from attribution tasks. Br J Psychiatry. 1994;164(5):637–646. | ||
Freeman D, Garety P, Fowler D, et al. The London-East Anglia randomized controlled trial of cognitive-behaviour therapy for psychosis. IV: Self-esteem and persecutory delusions. Br J Clin Psychol. 1998;37(Pt 4):415–430. | ||
Bentall RP, Kaney S. Content specific information processing and persecutory delusions: an investigation using the emotional Stroop test. Br J Med Psychol. 1989;62(Pt 4):355–364. | ||
Moritz S, Werner R, von Collani G. The inferiority complex in paranoia readdressed: a study with the Implicit Association Test. Cogn Neuropsychiatry. 2006;11(4):402–415. | ||
McKay R, Langdon R, Coltheart M. The defensive function of persecutory delusions: an investigation using the Implicit Association Test. Cogn Neuropsychiatry. 2007;12(1):1–24. | ||
Vázquez C, Diez-Alegría C, Hernández-Lloreda MJ, Moreno MN. Implicit and explicit self-schema in active deluded, remitted deluded, and depressed patients. J Behav Ther Exp Psychiatry. 2008;39(4):587–599. | ||
Kesting ML, Mehl S, Rief W, Lindenmeyer J, Lincoln TM. When paranoia fails to enhance self-esteem: explicit and implicit self-esteem and its discrepancy in patients with persecutory delusions compared to depressed and healthy controls. Psychiatry Res. 2011;186(2–3):197–202. | ||
Mackinnon K, Newman-Taylor K, Stopa L. Persecutory delusions and the self: An investigation of implicit and explicit self-esteem. J Behav Ther Exp Psychiatry. 2011;42(1):54–64. | ||
Valiente C, Cantero D, Vázquez C, Sanchez Á, Provencio M, Espinosa R. Implicit and explicit self-esteem discrepancies in paranoia and depression. J Abnorm Psychol. 2011;120(3):691–699. | ||
Bosson JK, Swann WB, Pennebaker JW. Stalking the perfect measure of implicit self-esteem: the blind men and the elephant revisited? J Pers Soc Psychol. 2000;79(4):631–643. | ||
Chadwick PD, Trower P, Juusti-Butler TM, Maguire N. Phenomenological evidence for two types of paranoia. Psychopathology. 2005;38(6):327–333. | ||
van der Gaag M. A neuropsychiatric model of biological and psychological processes in the remission of delusions and auditory hallucinations. Schizophr Bull. 2006;32 Suppl 1:S113–S122. | ||
The ICD-10 Classification of Mental and Behavioural Disorders: Clinical descriptions and diagnostic guidelines. Geneva: World Health Organization. Available from: http://www.who.int/classifications/icd/en/bluebook.pdf. Accessed May 1, 2014. | ||
Kolakowska T. Brief Psychiatric Rating Scale: Glossary and Rating Instruction. Oxford: Oxford University Press; 1976. | ||
Lachar D, Bailley SE, Rhoades HM, et al. New subscales for an anchored version of the Brief Psychiatric Rating Scale: construction, reliability, and validity in acute psychiatric admissions. Psychol Assess. 2001;13(3):384–395. | ||
Freeman D, Garety PA, Bebbington PE, et al. Psychological investigation of the structure of paranoia in a non-clinical population. Br J Psychiatry. 2005;186:427–435. | ||
Yamauchi T, Sudo A, Tanno Y. Factor structure and validity of Japanese-version Paranoia Checklist. Japanese Journal of Personality. 2008;17(2):182–193. | ||
Takahashi N, Tomita K, Higuchi T, Inada T. The inter-rater reliability of the Japanese version of the Montgomery-Asberg depression rating scale (MADRS) using a structured interview guide for MADRS (SIGMA). Hum Psychopharmacol. 2004;19(3):187–192. | ||
Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. | ||
Rosenberg M. Society and the Adolescent Self-image. Princeton, NJ: Princeton University Press; 1965. | ||
Mimura C, Griffiths P. A Japanese version of the Rosenberg Self-Esteem Scale: translation and equivalence assessment. J Psychosom Res. 2007;62(5):589–594. | ||
Sriram N, Greenwald AG. The Brief Implicit Association Test. Exp Psychol. 2009;56(4):283–294. | ||
Teachman BA, Woody SR. Automatic processing in spider phobia: implicit fear associations over the course of treatment. J Abnorm Psychol. 2003;112(1):100–109. | ||
Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85(2):197–216. | ||
Melo SS, Taylor JL, Bentall RP. ‘Poor me’ versus ‘bad me’ paranoia and the instability of persecutory ideation. Psychol Psychother. 2006;79(Pt 2):271–287. | ||
Karpinski A. Measuring self-esteem using the implicit association test: the role of the other. Pers Soc Psychol Bull. 2004;30(1):22–34. | ||
Flanagan P, Compton MT. A comparison of correlates of suicidal ideation prior to initial hospitalization for first-episode psychosis with prior research on correlates of suicide attempts prior to initial treatment seeking. Early Interv Psychiatry. 2012;6(2):138–144. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.