Back to Journals » Clinical Epidemiology » Volume 6
Cryptococcal meningitis: epidemiology and therapeutic options
Received 15 December 2013
Accepted for publication 7 February 2014
Published 13 May 2014 Volume 2014:6 Pages 169—182
DOI https://doi.org/10.2147/CLEP.S38850
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Derek J Sloan, Victoria Parris
Tropical and Infectious Disease Unit, Royal Liverpool University Hospital, Liverpool, UK
Abstract: Cryptococcal meningitis causes morbidity and mortality worldwide. The burden of disease is greatest in middle- and low-income countries with a high incidence of human immunodeficiency virus (HIV) infection. Patients taking immunosuppressive drugs and some immunocompetent hosts are also at risk. Treatment of cryptococcal meningitis consists of three phases: induction, consolidation, and maintenance. Effective induction therapy requires potent fungicidal drugs (amphotericin B and flucytosine), which are often unavailable in low-resource, high-endemicity settings. As a consequence, mortality is unacceptably high. Wider access to effective treatment is urgently required to improve outcomes. For human immunodeficiency virus-infected patients, judicious management of asymptomatic cryptococcal antigenemia and appropriately timed introduction of antiretroviral therapy are important.
Keywords: cryptococcosis, HIV, immunosuppression, antifungal therapy, immune reconstitution inflammatory syndrome, antiretroviral therapy
Introduction
Cryptococcosis is an important infectious disease globally. The majority of illness is among patients with defective cell-mediated immunity. Human immunodeficiency virus (HIV) infection is the main risk factor, accounting for 95% of cases in middle- and low-income countries (MLICs)1 and 80% of cases in high-income countries (HICs).2 Individuals taking immunosuppressive drugs (eg, transplant recipients) constitute most of the remaining caseload, although immunocompetent hosts are susceptible in some settings.
The most common clinical presentation is cryptococcal meningitis (CM), with over 1 million cases and 600,000 deaths per year.3 Nonmeningeal (eg, pulmonary and cutaneous) presentations also occur,4 and bloodstream infection (cryptococcemia) may disseminate to multiple sites.5
This review describes the epidemiology and management of cryptococcal disease. Worldwide distribution of the pathogen is outlined, incidence trends in patients with varying risk factors are assessed, and the prognostic implications of differing treatment protocols are highlighted.
Epidemiology of the infectious pathogen
Cryptococci are encapsulated saprophytic yeasts. Two species, transmitted by inhalation, are the principal human pathogens: Cryptococcus neoformans and Cryptococcus gattii.6 C. neoformans was identified by Sanfelice in 1894,7,8 and may be divided into two subtypes on the basis of capsular agglutination assays.9 C. neoformans var. grubii (capsular serotype D) is the most common, and causes 82% of cryptococcal disease worldwide. Var. neoformans (capsular serotype A) is responsible for 20%–30% of HIV-associated CM in northern Europe (notably France, Italy, and Denmark),9–11 but is less common in other global regions.12,13 Although both subtypes predominantly cause disease in immunocompromised individuals, several reports from the US14 and Asia15 suggest that var. grubii cryptococcosis in patients with normal immune systems is more common than previously assumed. The environmental reservoir of both subtypes is avian guano, decaying organic matter, and soil.8,16
C. gattii is traditionally associated with illness in immunocompetent individuals17–19 from tropical and subtropical regions, including Thailand,20 northern Australia,21,22 New Zealand, and Papua New Guinea.23–26 More recently, four molecular subtypes of C. gattii have been identified with distinct epidemiological characteristics that challenge this perspective.6 Whilst VGI (var gattii I) is the main subtype in Australasia, an outbreak of disease attributable to VGII has been described in immunocompetent patients from British Columbia, Canada.27–29 Between 1999 and 2010, 218 cases were identified on Vancouver Island.30,31 In 2006, a further case was reported on Orcas Island, Washington, USA,32 and C. gattii is now endemic throughout the Pacific Northwest of the US.29 Sporadic disease has also been notified in other parts of North America, including Florida, North Carolina, Rhode Island, New Mexico, Michigan, Georgia, and Montana.33 Additionally, C. gattii subtypes VGIII and -IV are more likely to be found in HIV-infected than immunocompetent patients. These strains may account for 2.4%–30% of HIV-associated cryptococcosis in some parts of Central and South America6 and southern Africa.34–37 The burden of human disease due to C. gattii is probably underrecognized, as many laboratories do not undertake detailed speciation of cryptococci.6
The environmental reservoirs of C. gattii are incompletely understood. In Australia, India, and other Asian countries, it has been isolated in eucalyptus trees.38 In British Columbia, it has been isolated from noneucalyptus tree species, soil, air, freshwater, and seawater.29 Discovery of this organism in heterogeneous biogeoclimatic zones suggests that its ecological niche was previously underestimated or that its distribution is expanding.39,40 Possible explanations for a changing distribution include climate change or altered land-use practices, such as logging.
HIV as a risk factor
The largest influence on the epidemiology of cryptococcal disease over the last 30 years has been the evolution of the HIV pandemic. Figure 1 shows that a fivefold increase in the incidence of cryptococcosis in France from 1985 to 1993 was almost entirely due to burgeoning disease in HIV-infected patients, while the number of cases in HIV-uninfected patients remained stable.41 Similar trends were observed in other HICs. In the UK, the number of annual cryptococcal case notifications rose from 13 (8% HIV-associated) in 1982 to 66 (83% HIV-associated) in 1991.42 Of 517 cryptococcal infections in New York City in 1991, 96% were HIV-related.43
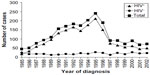  | Figure 1 Evolution of the incidence of cryptococcosis, by year of diagnosis in France (1985–2001), as reported to the National Reference Centre for Mycosis. |
HIV-infected patients are mainly at risk of cryptococcosis when they become very immunosuppressed and their CD4 count drops below 100 cells/μL.44,45 Consequentially, Figure 1 indicates that after the development of effective combination antiretroviral therapy (ART) in 1997, the upsurge in new cases of cryptococcal disease from HICs was reversed and incidence began to decline.46–48 From 1997–2001, France saw a 46% decrease in cases,41 from 1996 to 2007, incidence per 1,000 persons in the UK fell from three to 0.2,49 and from 1992 to 2000, incidence per 1,000 persons in Atlanta, Georgia, USA fell from 66 to seven.50
Figure 2 shows that disease trends in MLICs have been much worse. It is well recognized that sub-Saharan Africa has been the global region most heavily affected by HIV, with an estimated 2.6 million new infections per year at the peak of the epidemic in 1997.51 Contemporaneously, in the 1990s, CM became the leading cause of adult meningitis in many African countries, including Malawi (27% of cases),52 Zimbabwe (45% of cases),53,54 and South Africa (31% of cases).55 Delayed and incomplete access to ART meant that unlike Europe and North America, the incidence of CM did not recede after the turn of the millennium; a tertiary referral hospital in Botswana described C. neoformans growth from 15% of all cerebrospinal fluid (CSF) samples submitted for analysis in 2003,56 and a report from Cape Town, South Africa noted that CM still accounted for 31% of all inpatient days in new ART patients in 2007.57 A similar persistent elevation of the cryptococcal disease burden since the 1990s has been described from MLICs in Southeast Asia56,58 and Latin America.59
In addition to disparities in incidence between HICs and MLICs, there are well-documented differences in outcomes (Figure 2).3 A combination of earlier access to ART and availability of fungicidal drugs has contributed to falling mortality in HICs,2,60,61 while the death rate in MLICs has been relentlessly high.62 Analysis of pooled data from case series, surveillance reports, and clinical trials has estimated that the 90-day case-fatality rate from HIV-associated CM in East Asia, Oceania, Western Europe and the US is 9%, compared with 55% in other parts of Asia and South America and 70% in sub-Saharan Africa.3 Even acknowledging that some North American studies exclude the sickest patients,63 and some studies in MLICs show better case-fatality rates than others,64–67 these results are unacceptable.
  | Figure 2 Global incidence and mortality from cryptococcal meningitis among United Nations global regions from 1997 to 2007. |
Other risk factors
Although HIV is the largest driver of cryptococcal disease, it is important to acknowledge other factors. Prior to the HIV era in the UK, the incidence of cryptococcosis per 1,000 persons increased from 1.4 in 1963–1968 to 7.4 in 1973–1978.68 This was predominantly attributable to disease in patients on immunosuppressive medications. Use of potent immunosuppressants (eg, corticosteroids, calcineurin inhibitors,69 cytotoxic agents,70 and monoclonal antibodies71,72) for transplant conditioning or treatment of cancer and inflammatory conditions has continued to expand in HICs over the last 30 years, sustaining a small but important minority of cryptococcal illness in settings where HIV-related cases are in decline.73
Cryptococcosis disease occurs after 2.8%–8% of solid-organ transplants, and is the third-commonest invasive fungal infection in this setting, after Candida and Aspergillus.69,74 In a retrospective review of US data from 1996 to 2010, kidney-transplant recipients were most often affected, followed by liver, heart, lung, and pancreas recipients.5 The median time to diagnosis after solid-organ transplantation is 20 months, and the etiology is normally reactivation of latent disease.5,74,75 Symptoms may emerge sooner after lung or liver transplants, perhaps because the required level of postoperative immunosuppression is higher.69 The overall likelihood of cryptococcal disease does not vary between patients using tacrolimus, cyclosporine, or azathioprine as the primary immunosuppressive agent, but patients who are coadministered high-dose corticosteroids may be at higher risk.5
Infrequently, cryptococcal infection is acquired from donor tissue. This is particularly suspected if disease occurs within 30 days of transplantation, at surgical graft sites, or in multiple organ recipients of a single donor.75–77 Screening of donors is not routinely performed, but should be undertaken if the donor has unexplained pulmonary lesions, undiagnosed neurological illness, or unexplained fever with relevant comorbid risk factors.76,77
Cryptococcal disease is rare following hematopoietic stem cell transplant or corneal tissue transplant.78 Data from a consortium of US transplant centers (Transplant-Associated Infection Surveillance Network) revealed an incidence of only 0.6% in hematopoietic stem cell-transplant recipients between 2001 and 2006.79,80 For unknown reasons, the risk is higher in autologous than allogenic transplants.78
Non-HIV-infected, nontransplant recipients with cryptococcosis are a heterogeneous group. Except for C. gattii outbreaks in immunocompetent hosts, most patients have immune dysfunction related to the pathophysiology or treatment of an underlying autoimmune disease, malignancy, or innate immunological disorder. It is difficult to generalize about these cases, but in HICs they tend to experience higher mortality than their HIV-infected counterparts. The reasons for this include the effects of underlying illness and late diagnosis, because the pathogen was not initially suspected.5,73,81
Clinical presentation
Epidemiological variables, including the nature of immunosuppressive risk factors and pathogen species, influence the presentation of cryptococcal disease. CM is the leading presentation overall,19,41,42,78 but nonmeningeal manifestations are proportionally more frequent in non-HIV-infected individuals.5,42,73,82 Transplant-associated cryptococcosis is often limited to the lungs,83,84 with disseminated or neurological disease in 52%–61% of cases.69,84
Presentation of C. gattii infection in immunocompetent hosts varies according to molecular subtype. In Australia, where the majority of disease is due to VGI, CM is most common,6,85 but in North America, VGII disease presents with respiratory symptoms in 76%, neurological symptoms in 7.8%, and both respiratory and neurological symptoms in 10.1% of cases.19,24,31
The commonest features of CM are subacute headache and confusion. Intracranial pressure (ICP) is often elevated, and may cause cranial nerve palsies or seizures. Classical features of “meningism” (eg, neck stiffness) occur in less than 20% of patients.86 Altered mental state is associated with higher mortality.5,50,87
Neurological infection may be complicated by mass lesions (cryptococcomas). This is more common with C. gattii than C. neoformans. Clinical sequelae of cryptococcomas include hydrocephalus and blindness.88,89 Some patients require neurosurgical intervention.17,18
Forty percent of patients with CM have ocular involvement, including papilledema and uveitis with multifocal chorioretinitis.90,91 Immune-mediated optic nerve dysfunction and blindness have been particularly reported amongst C. gattii patients from Papua New Guinea.54,89,92 The spectrum of pulmonary illness ranges from asymptomatic colonization to severe, progressive pneumonia and cryptococcomas in the lungs. Skin lesions often contain the infecting organism. In severely immunocompromised individuals, disseminated disease (involvement of two or more sites) may present as fever and rash before other symptoms and signs appear.
Investigations
Confirmation of CM requires lumbar puncture (LP) and examination of CSF, as shown in Figure 3A. Lack of LP equipment may result in underestimation of the disease burden in MLICs.93 Typical CSF features include a raised opening pressure (reflecting elevated ICP), lymphocytic pleocytosis, and evidence of inflammation. However, CSF may be normal in 10%–17% of patients,54,94 especially in HIV-endemic populations.5 Identification of the infecting organism is traditionally done by light microscopy after India ink staining, but this method is user-dependent with variable sensitivity. Detection of cryptococcal antigen (CrAg) by a latex-agglutination test63 or lateral flow immunoassay (LFA) is better (Figure 3B). The lateral flow immunoassay is cheaper than latex agglutination,95,96 and may be applied to urine samples when CSF is unobtainable.97,98 Fungal culture of CSF on Sabouraud media is required to isolate the organism for antimicrobial susceptibility testing. Characteristic colonies grow after 36 hours (Figure 3C).
Radiology has little role in the diagnosis of CM, but computed tomography and magnetic resonance imaging scans are necessary to detect complications (eg, cryptococcomas and noncommunicating hydrocephalus). These modalities are generally unavailable in MLICs.
Nonmeningeal cryptococcosis may be confirmed by tissue sampling for microbiological analysis. Cryptococcemia is identified from fungal blood cultures or CrAg detection in serum samples. Asymptomatic antigenemia (a positive serum CrAg in the absence of clinical disease) has been described in HIV-infected patients, and may predict impending CM. Screening and treatment for asymptomatic antigenemia will be discussed later.
Treatment and prognosis
The Infectious Diseases Society of America (IDSA)4 and World Health Organization (WHO)99 have recently issued updated treatment guidelines to reflect advances over the last decade, but routine practice in MLICs continues to be impeded by poor drug availability. Figure 4 summarizes current recommendations.
Induction and consolidation antifungal therapy for HIV-associated CM
CM treatment consists of three phases: induction, consolidation, and maintenance. IDSA and WHO guidelines emphasize the importance of potent fungicidal drugs during induction therapy, because the rate of fungal clearance from the CSF during the first 2 weeks, known as early fungicidal activity (EFA),100 predicts 10-week survival,101 and CSF sterilization by 14 days predicts long-term prognosis.63
Amphotericin B (AmB), the drug with the greatest EFA, is administered intravenously for 14 days during induction therapy whenever possible. Its activity is concentration-dependent,102 but the required dose (0.7–1.0 mg/kg) of the commonest preparation (AmB deoxycholate [AmBd])33,63–65 can be nephrotoxic.103,104 A solution in HICs is the use of lipid drug formulations with fewer renal side effects, including liposomal AmB (LAmB; 3–6 mg/kg/day) and AmB lipid complex (ABLC, 5 mg/kg/day).105–107 The cost of these (over US$1,000 per day108) is prohibitive for MLICs, so alternative strategies, including preemptive hydration and electrolyte supplementation, have been developed to minimize the toxicity of AmBd.99 Studies in Kampala,62 Cape Town,65 and Bangkok109 support this approach.
Even a 2-week course of AmBd (US$12–$15 per day) is too expensive for some LICs.110 In this scenario, data from South Africa and Malawi have demonstrated that 5–7 days of AmBd is better than treatment that is restricted to less fungicidal drugs.64,111 AmBd-treated patients who survive the first 6 months have a subsequent 5-year survival rate of 88%.112 This advocates for investment in early AmBd to achieve satisfactory long-term outcomes.
Flucytosine should accompany AmB during induction therapy at an intravenous or oral dose of 100 mg/kg/day.100,113–115 Omission of this agent has been associated with higher rates of mortality,113 treatment failure,116 and late relapse.117 Toxic cytopenias can occur during flucytosine therapy, and so regular full blood counts and therapeutic drug monitoring (TDM) are advised by IDSA guidelines.4,57,118 TDM is arduous, and the absolute need for it in MLICs was questioned by a recent study in Vietnam that did not use TDM but demonstrated safe and effective use of AmBd-flucytosine.113
Despite its value, flucytosine remains unlicensed in most African and Asian countries,114,119,120 so alternative agents have been considered for combination with AmB. The obvious contender is fluconazole, which is freely distributed in MLICs (http://www.pfizer.com/responsibility/global_health/diflucan_partnership_program), but is fungistatic rather than fungicidal in the normal human dose range. Definitive evidence to support AmB-fluconazole induction therapy is lacking, but reports from several countries describe rapid EFA when intravenous AmBd (0.7–1 mg/kg/day) is prescribed alongside oral fluconazole (800–1,200 mg/day).109,113,121,122 A meta-analysis of various induction strategies in resource-poor settings has described AmBd-fluconazole as cost-effective.123 The WHO recommends this approach when flucytosine cannot be obtained.99
After a 14-day induction phase, treatment proceeds with a consolidation phase of 400 mg once daily (od) for a further 8 weeks. This dose may be increased to 800 mg when gold-standard induction therapy with AmB-flucytosine is unavailable.
Gaps in drug provision leave fluconazole as the only agent for induction and consolidation therapy in many high-burden countries, contributing to significant variation in prognosis. The response to this requires discussion. Until recently, the routine dose of fluconazole for CM monotherapy was 200–400 mg od, and 8-week mortality was 78%–90%.86,124 In one South African study from 2006, median patient survival on induction- and consolidation-phase fluconazole (400 mg od) was only 76 days.125
Such poor outcomes prompted dose escalation. Clinical studies in Uganda and Malawi based on 800 mg od induction and 400 mg od consolidation therapy reported improved 10-week mortality rates of 58%–60%.87,126 A further induction-phase dose increase to 1,200 mg was associated with faster EFA126 but did not improve survival,126,127 and a pharmacokinetic–pharmacodynamic bridging study from a mouse model indicated that 1,200 mg od will fail to achieve fungal stasis in the CSF of 33% of patients.128 An exploratory clinical trial has suggested that induction with 1,600–2,000 mg of fluconazole would be more efficacious,126,129 but additional evaluation of these doses is required. WHO guidelines currently advocate that where fluconazole monotherapy is the only option, 1,200 mg od should be used for 2-week induction therapy followed by a consolidation phase of 800 mg od for 8 weeks.99
A final option when intravenous drug administration is not feasible is a fully oral induction phase of fluconazole and flucytosine. Trials in Malawi have confirmed that fluconazole (1,200 mg od) and flucytosine (100 mg/kg/day) achieve faster EFA and lower 10-week mortality than fluconazole alone,70,111,127 suggesting that fluconazole monotherapy should be augmented by induction-phase flucytosine wherever possible.
Overall, reduced availability of fungicidal drugs continues to compromise outcomes in high-burden countries. An ongoing multicenter clinical trial (Advancing Cryptococcal meningitis Treatment in Africa [ACTA]130) in sub-Saharan Africa hopes to confirm the shortest, simplest effective regimens, but will require backup by universal provision of medicines for routine care.
Maintenance antifungal therapy for HIV-associated CM
After consolidation therapy, secondary prophylaxis with fluconazole (200 mg od) minimizes the risk of CM relapse.131 Alternative, less effective maintenance regimens include oral itraconazole (200 mg od)117 and intravenous AmBd (1 mg/kg/once weekly).132
The required duration of maintenance therapy has recently been examined, particularly as the 1-year default rate from secondary prophylaxis in some African settings exceeds 90%.133,134 In the pre-ART era, lifelong fluconazole was recommended after a presentation with CM, but it now appears that late relapse is unlikely during successful ART.135–138 International guidelines state that immune restoration by ART permits discontinuation of maintenance therapy (Figure 4). However, evidence to support cessation of secondary prophylaxis is weaker when induction/consolidation therapy is not fungicidal (eg, fluconazole monotherapy), and isolated CM relapses have been described in patients on ART with CD4 counts up to 495 cells/μL.139
Differences in antifungal therapy for non-HIV-associated CM
Treatment of non-HIV-associated CM varies from that described above, dependent on characteristics of the host and pathogen (Figure 4). Patients developing CM after solid-organ transplant often take nephrotoxic immunosuppressants (tacrolimus, cyclosporine or sirolimus) to prevent graft rejection, and 25% of transplant recipients have renal dysfunction at CM diagnosis. Therefore, kidney-friendly liposomal preparations of AmB (eg, LAmB or ABLC) are recommended during induction therapy.4 It is uncertain whether immunosuppressive therapy should be stopped during CM treatment; this may accelerate eradication of the pathogen, but poses a risk of proinflammatory immune reconstitution syndrome or transplant rejection.140 Although clear evidence is lacking, some authors report good outcomes with a staged reduction in immunosuppressive therapy alongside antifungal drugs.141
Secondary fluconazole prophylaxis in transplant recipients may stop after 6–12 months, as the late cryptococcal relapse rate is only 1%–3%.142 There is no standard regimen for non-HIV, nontransplant patients with CM. Some authors advocate a longer (4–6 weeks) induction phase of AmB/flucytosine (Figure 4), while others favor a standard 2-week induction phase. Consolidation and maintenance therapy are identical to transplant recipients. C. gattii infection should be treated with the same drugs as C. neoformans, but the response to therapy may be slower, due to higher azole minimum inhibitory concentrations143,144 and poor drug penetration of cryptococcomas.17,18,85
Asymptomatic antigenemia and primary prophylaxis
Between 4% and 20% of patients with newly identified HIV infection and a CD4 count <150 cells/μL have a positive serum CrAg test in the absence of clinical cryptococcosis.145–147 Asymptomatic antigenemia predicts impending CM,148 and is associated with increased mortality.149 Serum CrAg screening of new HIV patients is being implemented in South Africa,150 prompting debate on the use of preemptive therapy for those at highest risk.
Treatment of asymptomatic antigenemia is not recommended in HICs,4 but some studies support fluconazole therapy for serum CrAg-positive patients in MLICs.151–153 A management algorithm is shown in Figure 5.154 However, deployment of preventive screening and therapy strategies is operationally difficult, and an implementation study in Kenya achieved effective fluconazole administration for only 52% of eligible patients.155 The benefit of presumptive therapy for asymptomatic antigenemia will depend on the logistics of integrating this strategy into routine practice at ART clinics.
  | Figure 5 A screening and management strategy for asymptomatic antigenemia. |
An alternative means of CM prevention is primary prophylaxis with fluconazole for all patients with CD4 counts <100 cells/μL, irrespective of serum CrAg testing. Studies of this approach in Thailand156 and Uganda157 demonstrated that fluconazole 200 mg once daily reduced the incidence of CM, but there was no reduction in overall mortality and rates of fluconazole-resistant Candida albicans infection increased.158 The cost-effectiveness of no preventive treatment, therapy for asymptomatic antigenemia, or primary prophylaxis is likely to vary between regions, based on the underlying epidemiology of cryptococcal infection and availability of ART.
Additional therapeutic considerations
Outcomes from CM may be improved by reduction of raised ICP during early therapy, careful management of immune reconstitution inflammatory syndrome (IRIS) and appropriately timed ART initiation for HIV-infected patients.
Reducing raised intracranial pressure
Increased ICP (>25 cm/H2O) is associated with greater CSF fungal burden159 and higher mortality.160 Regular CSF drainage by serial LPs is recommended.115,161–164 Insertion of a temporary CSF-drainage catheter165 or ventriculoperitoneal shunt may also be used.166 Drug therapy (eg, acetazolamide or corticosteroids) to reduce CSF pressure or prevent blindness in CM patients is not beneficial, and acetazolamide may cause harm.88,160,167
Managing immune reconstitution inflammatory syndromes
IRIS in CM patients occurs when host immune recovery triggers inflammatory reactions to persistent fungal antigens. There are two main forms: unmasking and paradoxical (Figure 6).168
Unmasking IRIS occurs in HIV-infected patients when subclinical cryptococcal disease emerges after ART is commenced. This might be prevented by careful pre-ART screening. However, late ART is generally associated with lower survival,169 and patients who are already on HIV therapy when they present with CM tend to have better outcomes,64,170 so excessive delays should be avoided.
Paradoxical IRIS is best described in HIV-associated CM patients who initially respond to antifungal drugs and then deteriorate within 12 months of starting ART. Studies from South Africa and Ethiopia estimate an incidence of 7%–33%.171–173 Paradoxical IRIS also affects solid organ-transplant patients when antirejection medications are interrupted during CM therapy,141 and apparently healthy hosts may suffer from reactivation of immune defenses that were previously overwhelmed by high fungal burden.
Paradoxical IRIS in the central nervous system has a mortality of up to 36%.174,175 Risk factors include severe disease at presentation and slow fungal elimination.176,177 The benefit of anti-inflammatory drugs (eg, corticosteroids100) is unproven.178 Highly fungicidal induction-phase therapy and rapid CSF sterilization is the best way to minimize unwanted reactions.179,180
Combining anticryptococcal and anti-HIV medications
In HIV-associated CM, IRIS is more likely during immune reconstitution from lower baseline CD4 counts, and is influenced by the timing of ART introduction. Balancing the danger of early mortality from advanced immunosuppression against that of accelerated immune recovery is difficult, and best practice remains to be established. A retrospective study of mortality after ART initiation in Thailand at time points 1–12 months into CM therapy did not show any association between timing of ART and outcome.181 Table 1 summarizes subsequent prospective trials.135,136,182–185 The most convincing data come from a recent study in Uganda and South Africa, which was terminated early because ART initiation within the first 28 days of CM treatment led to a higher risk of IRIS and death.185 Introduction of ART 4–10 weeks after starting antifungal treatment is currently considered the safest approach.
Conclusion
Advanced HIV infection continues to drive cryptococcal disease worldwide. Patients on immunosuppressive drugs and some immunocompetent hosts are also at risk. Although treatment with potent drug combinations provides effective cure, poor availability of fungicidal drugs in MLICs results in high case-fatality rates. Expanded provision of fungicidal treatment is urgently required. Ongoing research on management of asymptomatic antigenemia and optimal timing of ART initiation is important to improve the prognosis of HIV-associated CM.
Disclosure
The authors report no conflicts of interest in this work.
References
Leal AL, Faganello J, Fuentefria AM, Boldo JT, Bassanesi MC, Vainstein MH. Epidemiological profile of cryptococcal meningitis patients in Rio Grande do Sul, Brazil. Mycopathologia. 2008;166:71–75. | |
Pyrgos V, Seitz AE, Steiner CA, Prevots DR, Williamson PR. Epidemiology of cryptococcal meningitis in the US: 1997–2009. PLoS One. 2013;8:e56269. | |
Park BJ, Wannemuehler KA, Marston BJ, Govender N, Pappas PG, Chiller TM. Estimation of the current global burden of cryptococcal meningitis among persons living with HIV/AIDS. AIDS. 2009;23:525–530. | |
Perfect JR, Dismukes WE, Dromer F, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322. | |
Brizendine KD, Baddley JW, Pappas PG. Predictors of mortality and differences in clinical features among patients with cryptococcosis according to immune status. PLoS One. 2013;8:e60431. | |
Byrnes EJ 3rd, Bartlett KH, Perfect JR, Heitman J. Cryptococcus gattii: an emerging fungal pathogen infecting humans and animals. Microbes Infect. 2011;13:895–907. | |
Sanfelice F. Sull’azione patogena dei bastomiceti [On the action of pathogenic bastomiceti]. Ann Isto Igiene R Univ Roma. 1895;5:239–262. Italian. | |
Sanfelice F. Contributo alle morfologia e biologia dei blastomiceti che si sviluppano nei succhi di alcuni frutti [Contribution to the morphology and biology of blastomiceti developing in some fruit juices]. Ann Isto Igiene R Univ Roma. 1894;4:463–495. Italian. | |
Franzot SP, Salkin IF, Casadevall A. Cryptococcus neoformans var. grubii: separate varietal status for Cryptococcus neoformans serotype A isolates. J Clin Microbiol. 1999;37:838–840. | |
Dromer F, Mathoulin S, Dupont B, Letenneur L, Ronin O. Individual and environmental factors associated with infection due to Cryptococcus neoformans serotype D. French Cryptococcosis Study Group. Clin Infect Dis. 1996;23:91–96. | |
Tortorano AM, Viviani MA, Rigoni AL, Cogliati M, Roverselli A, Pagano A. Prevalence of serotype D in Cryptococcus neoformans isolates from HIV positive and HIV negative patients in Italy. Mycoses. 1997;40:297–302. | |
Antinori S. New Insights into HIV/AIDS-associated cryptococcosis. ISRN AIDS. 2013;2013:471363. | |
Kwon-Chung KJ, Bennett JE. Epidemiologic differences between the two varieties of Cryptococcus neoformans. Am J Epidemiol. 1984;120:123–130. | |
Pappas PG, Perfect JR, Cloud GA, et al. Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis. 2001;33:690–699. | |
Lui G, Lee N, Ip M, et al. Cryptococcosis in apparently immunocompetent patients. QJM. 2006;99:143–151. | |
Velagapudi R, Hsueh YP, Geunes-Boyer S, Wright JR, Heitman J. Spores as infectious propagules of Cryptococcus neoformans. Infect Immun. 2009;77:4345–4355. | |
Mitchell DH, Sorrell TC, Allworth AM, et al. Cryptococcal disease of the CNS in immunocompetent hosts: influence of cryptococcal variety on clinical manifestations and outcome. Clin Infect Dis. 1995;20:611–616. | |
Speed B, Dunt D. Clinical and host differences between infections with the two varieties of Cryptococcus neoformans. Clin Infect Dis. 1995;21:28–34; discussion 5–6. | |
Chen SC, Slavin MA, Heath CH, et al. Clinical manifestations of Cryptococcus gattii infection: determinants of neurological sequelae and death. Clin Infect Dis. 2012;55:789–798. | |
Sukroongreung S, Nilakul C, Ruangsomboon O, Chuakul W, Eampokalap B. Serotypes of Cryptococcus neoformans isolated from patients prior to and during the AIDS era in Thailand. Mycopathologia. 1996;135:75–78. | |
Fisher D, Burrow J, Lo D, Currie B. Cryptococcus neoformans in tropical northern Australia: predominantly variant gattii with good outcomes. Aust N Z J Med. 1993;23:678–682. | |
Ellis DH. Cryptococcus neoformans var. gattii in Australia. J Clin Microbiol. 1987;25:430–431. | |
Seaton RA. The management of cryptococcal meningitis in Papua New Guinea. P N G Med J. 1996;39:67–73. | |
Seaton RA, Hamilton AJ, Hay RJ, Warrell DA. Exposure to Cryptococcus neoformans var. gattii – a seroepidemiological study. Trans R Soc Trop Med Hyg. 1996;90:508–512. | |
Laurenson IF, Lalloo DG, Naraqi S, et al. Cryptococcus neoformans in Papua New Guinea: a common pathogen but an elusive source. J Med Vet Mycol. 1997;35:437–440. | |
Laurenson IF, Trevett AJ, Lalloo DG, et al. Meningitis caused by Cryptococcus neoformans var. gattii and var. neoformans in Papua New Guinea. Trans R Soc Trop Med Hyg. 1996;90:57–60. | |
Kidd SE, Hagen F, Tscharke RL, et al. A rare genotype of Cryptococcus gattii caused the cryptococcosis outbreak on Vancouver Island (British Columbia, Canada). Proc Natl Acad Sci U S A. 2004;101:17258–17263. | |
Fraser JA, Giles SS, Wenink EC, et al. Same-sex mating and the origin of the Vancouver Island Cryptococcus gattii outbreak. Nature. 2005;437:1360–1364. | |
Datta K, Bartlett KH, Baer R, et al. Spread of Cryptococcus gattii into Pacific Northwest region of the United States. Emerg Infect Dis. 2009;15:1185–1191. | |
Centers for Disease Control and Prevention. Emergence of Cryptococcus gattii – Pacific Northwest, 2004–2010. MMWR Morb Mortal Wkly Rep. 2010;59:865–868. | |
Bartlett KH, Cheng PY, Duncan C, et al. A decade of experience: Cryptococcus gattii in British Columbia. Mycopathologia. 2012;173:311–319. | |
Upton A, Fraser JA, Kidd SE, et al. First contemporary case of human infection with Cryptococcus gattii in Puget Sound: evidence for spread of the Vancouver Island outbreak. J Clin Microbiol. 2007;45:3086–3088. | |
Brandt ME, Hutwagner LC, Klug LA, et al. Molecular subtype distribution of Cryptococcus neoformans in four areas of the United States. Cryptococcal Disease Active Surveillance Group. J Clin Microbiol. 1996;34:912–917. | |
Karstaedt AS, Crewe-Brown HH, Dromer F. Cryptococcal meningitis caused by Cryptococcus neoformans var. gattii, serotype C, in AIDS patients in Soweto, South Africa. Med Mycol. 2002;40:7–11. | |
McCarthy KM, Morgan J, Wannemuehler KA, et al. Population-based surveillance for cryptococcosis in an antiretroviral-naive South African province with a high HIV seroprevalence. AIDS. 2006;20:2199–2206. | |
Steele KT, Thakur R, Nthobatsang R, Steenhoff AP, Bisson GP. In-hospital mortality of HIV-infected cryptococcal meningitis patients with C. gattii and C. neoformans infection in Gaborone, Botswana. Med Mycol. 2010;48:1112–1115. | |
Litvintseva AP, Thakur R, Reller LB, Mitchell TG. Prevalence of clinical isolates of Cryptococcus gattii serotype C among patients with AIDS in sub-Saharan Africa. J Infect Dis. 2005;192:888–892. | |
Pfeiffer TJ, Ellis DH. Environmental isolation of Cryptococcus neoformans var. gattii from Eucalyptus tereticornis. J Med Vet Mycol. 1992;30:407–408. | |
Bartlett KH, Kidd SE, Kronstad JW. The emergence of Cryptococcus gattii in British Columbia and the Pacific Northwest. Curr Infect Dis Rep. 2008;10:58–65. | |
MacDougall L, Kidd SE, Galanis E, et al. Spread of Cryptococcus gattii in British Columbia, Canada, and detection in the Pacific Northwest, USA. Emerg Infect Dis. 2007;13:42–50. | |
Dromer F, Mathoulin-Pelissier S, Fontanet A, Ronin O, Dupont B, Lortholary O. Epidemiology of HIV-associated cryptococcosis in France (1985–2001): comparison of the pre- and post-HAART eras. AIDS. 2004;18:555–562. | |
Knight FR, Mackenzie DW, Evans BG, Porter K, Barrett NJ, White GC. Increasing incidence of cryptococcosis in the United Kingdom. J Infect. 1993;27:185–191. | |
Currie BP, Casadevall A. Estimation of the prevalence of cryptococcal infection among patients infected with the human immunodeficiency virus in New York City. Clin Infect Dis. 1994;19:1029–1033. | |
Jarvis JN, Harrison TS. HIV-associated cryptococcal meningitis. AIDS. 2007;21:2119–2129. | |
Kisenge PR, Hawkins AT, Maro VP, et al. Low CD4 count plus coma predicts cryptococcal meningitis in Tanzania. BMC Infect Dis. 2007;7:39. | |
van Elden LJ, Walenkamp AM, Lipovsky MM, et al. Declining number of patients with cryptococcosis in the Netherlands in the era of highly active antiretroviral therapy. AIDS. 2000;14:2787–2788. | |
Mocroft A, Vella S, Benfield TL, et al. Changing patterns of mortality across Europe in patients infected with HIV-1. EuroSIDA Study Group. Lancet. 1998;352:1725–1730. | |
Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. | |
Garvey L, Winston A, Walsh J, et al. HIV-associated central nervous system diseases in the recent combination antiretroviral therapy era. Eur J Neurol. 2011;18:527–534. | |
Mirza SA, Phelan M, Rimland D, et al. The changing epidemiology of cryptococcosis: an update from population-based active surveillance in 2 large metropolitan areas, 1992-2000. Clin Infect Dis. 2003;36:789–794. | |
Joint United Nations Programme on HIV/AIDS. World AIDS Day Report – 2011. Geneva: UNAIDS; 2011. Available from: http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/jc2216_worldaidsday_report_2011_en.pdf. Accessed February 13, 2014. | |
Gordon SB, Walsh AL, Chaponda M, et al. Bacterial meningitis in Malawian adults: pneumococcal disease is common, severe, and seasonal. Clin Infect Dis. 2000;31:53–57. | |
Heyderman RS, Gangaidzo IT, Hakim JG, et al. Cryptococcal meningitis in human immunodeficiency virus-infected patients in Harare, Zimbabwe. Clin Infect Dis. 1998;26:284–289. | |
Hakim JG, Gangaidzo IT, Heyderman RS, et al. Impact of HIV infection on meningitis in Harare, Zimbabwe: a prospective study of 406 predominantly adult patients. AIDS. 2000;14:1401–1407. | |
Schutte CM, Van der Meyden CH, Magazi DS. The impact of HIV on meningitis as seen at a South African academic hospital (1994 to 1998). Infection. 2000;28:3–7. | |
Bisson GP, Lukes J, Thakur R, Mtoni I, MacGregor RR. Cryptococcus and lymphocytic meningitis in Botswana. S Afr Med J. 2008;98:724–725. | |
Harling G, Orrell C, Wood R. Healthcare utilization of patients accessing an African national treatment program. BMC Health Serv Res. 2007;7:80. | |
Nissapatorn V. Lessons learned about opportunistic infections in Southeast Asia. Southeast Asian J Trop Med Public Health. 2008;39:625–641. | |
Leimann BC, Koifman RJ. Cryptococcal meningitis in Rio de Janeiro State, Brazil, 1994–2004. Cad Saude Publica. 2008;24:2582–2592. | |
Lortholary O, Poizat G, Zeller V, et al. Long-term outcome of AIDS-associated cryptococcosis in the era of combination antiretroviral therapy. AIDS. 2006;20:2183–2191. | |
Antinori S, Ridolfo A, Fasan M, et al. AIDS-associated cryptococcosis: a comparison of epidemiology, clinical features and outcome in the pre- and post-HAART eras. Experience of a single centre in Italy. HIV Med. 2009;10:6–11. | |
Kambugu A, Meya DB, Rhein J, et al. Outcomes of cryptococcal meningitis in Uganda before and after the availability of highly active antiretroviral therapy. Clin Infect Dis. 2008;46:1694–1701. | |
van der Horst CM, Saag MS, Cloud GA, et al. Treatment of cryptococcal meningitis associated with the acquired immunodeficiency syndrome. National Institute of Allergy and Infectious Diseases Mycoses Study Group and AIDS Clinical Trials Group. N Engl J Med. 1997;337:15–21. | |
Bicanic T, Meintjes G, Wood R, et al. Fungal burden, early fungicidal activity, and outcome in cryptococcal meningitis in antiretroviral-naive or antiretroviral-experienced patients treated with amphotericin B or fluconazole. Clin Infect Dis. 2007;45:76–80. | |
Bicanic T, Wood R, Meintjes G, et al. High-dose amphotericin B with flucytosine for the treatment of cryptococcal meningitis in HIV-infected patients: a randomized trial. Clin Infect Dis. 2008;47:123–130. | |
Pitisuttithum P, Tansuphasawadikul S, Simpson AJ, Howe PA, White NJ. A prospective study of AIDS-associated cryptococcal meningitis in Thailand treated with high-dose amphotericin B. J Infect. 2001;43:226–233. | |
Sloan DJ, Dedicoat MJ, Lalloo DG. Treatment of cryptococcal meningitis in resource limited settings. Curr Opin Infect Dis. 2009;22:455–463. | |
Hay RJ, Mackenzie DW, Campbell CK, Philpot CM. Cryptococcosis in the United Kingdom and the Irish Republic: an analysis of 69 cases. J Infect. 1980;2:13–22. | |
Husain S, Wagener MM, Singh N. Cryptococcus neoformans infection in organ transplant recipients: variables influencing clinical characteristics and outcome. Emerg Infect Dis. 2001;7:375–381. | |
Slavin MA, Chen SC. Cryptococcosis, lymphoproliferative disorders and modern day chemotherapy regimens. Leuk Lymphoma. 2013;54:449–450. | |
Hage CA, Wood KL, Winer-Muram HT, Wilson SJ, Sarosi G, Knox KS. Pulmonary cryptococcosis after initiation of anti-tumor necrosis factor-alpha therapy. Chest. 2003;124:2395–2397. | |
Nath DS, Kandaswamy R, Gruessner R, Sutherland DE, Dunn DL, Humar A. Fungal infections in transplant recipients receiving alemtuzumab. Transplant Proc. 2005;37:934–936. | |
Bratton EW, El Husseini N, Chastain CA, et al. Comparison and temporal trends of three groups with cryptococcosis: HIV-infected, solid organ transplant, and HIV-negative/non-transplant. PLoS One. 2012;7:e43582. | |
Neofytos D, Fishman JA, Horn D, et al. Epidemiology and outcome of invasive fungal infections in solid organ transplant recipients. Transpl Infect Dis. 2010;12:220–229. | |
Sun HY, Alexander BD, Lortholary O, et al. Unrecognized pretransplant and donor-derived cryptococcal disease in organ transplant recipients. Clin Infect Dis. 2010;51:1062–1069. | |
Baddley JW, Schain DC, Gupte AA, et al. Transmission of Cryptococcus neoformans by organ transplantation. Clin Infect Dis. 2011;52:e94–e98. | |
Singh N, Huprikar S, Burdette SD, Morris MI, Blair JE, Wheat LJ. Donor-derived fungal infections in organ transplant recipients: guidelines of the American Society of Transplantation, infectious diseases community of practice. Am J Transplant. 2012;12:2414–2428. | |
Sun HY, Wagener MM, Singh N. Cryptococcosis in solid-organ, hematopoietic stem cell, and tissue transplant recipients: evidence-based evolving trends. Clin Infect Dis. 2009;48:1566–1576. | |
Pappas PG, Alexander BD, Andes DR, et al. Invasive fungal infections among organ transplant recipients: results of the Transplant-Associated Infection Surveillance Network (TRANSNET). Clin Infect Dis. 2010;50:1101–1111. | |
Kontoyiannis DP, Marr KA, Park BJ, et al. Prospective surveillance for invasive fungal infections in hematopoietic stem cell transplant recipients, 2001–2006:overview of the Transplant-Associated Infection Surveillance Network (TRANSNET) database. Clin Infect Dis. 2010;50:1091–1100. | |
Nguyen MH, Husain S, Clancy CJ, et al. Outcomes of central nervous system cryptococcosis vary with host immune function: results from a multi-center, prospective study. J Infect. 2010;61:419–426. | |
Dromer F, Mathoulin S, Dupont B, Laporte A. Epidemiology of cryptococcosis in France: a 9-year survey (1985–1993). French Cryptococcosis Study Group. Clin Infect Dis. 1996;23:82–90. | |
Singh N, Alexander BD, Lortholary O, et al. Cryptococcus neoformans in organ transplant recipients: impact of calcineurin-inhibitor agents on mortality. J Infect Dis. 2007;195:756–764. | |
Shaariah W, Morad Z, Suleiman AB. Cryptococcosis in renal transplant recipients. Transplant Proc. 1992;24:1898–1899. | |
Chen S, Sorrell T, Nimmo G, et al. Epidemiology and host- and variety-dependent characteristics of infection due to Cryptococcus neoformans in Australia and New Zealand. Australasian Cryptococcal Study Group. Clin Infect Dis. 2000;31:499–508. | |
Mwaba P, Mwansa J, Chintu C, et al. Clinical presentation, natural history, and cumulative death rates of 230 adults with primary cryptococcal meningitis in Zambian AIDS patients treated under local conditions. Postgrad Med J. 2001;77:769–773. | |
Rothe C, Sloan DJ, Goodson P, et al. A prospective longitudinal study of the clinical outcomes from cryptococcal meningitis following treatment induction with 800 mg oral fluconazole in Blantyre, Malawi. PLoS One. 2013;8:e67311. | |
Seaton RA, Verma N, Naraqi S, Wembri JP, Warrell DA. The effect of corticosteroids on visual loss in Cryptococcus neoformans var. gattii meningitis. Trans R Soc Trop Med Hyg. 1997;91:50–52. | |
Seaton RA, Verma N, Naraqi S, Wembri JP, Warrell DA. Visual loss in immunocompetent patients with Cryptococcus neoformans var. gattii meningitis. Trans R Soc Trop Med Hyg. 1997;91:44–49. | |
Lesser RL, Simon RM, Leon H, Siegel N. Cryptococcal meningitis and internal ophthalmoplegia. Am J Ophthalmol. 1979;87:682–687. | |
Kestelyn P, Taelman H, Bogaerts J, et al. Ophthalmic manifestations of infections with Cryptococcus neoformans in patients with the acquired immunodeficiency syndrome. Am J Ophthalmol. 1993;116:721–727. | |
Lalloo D, Fisher D, Naraqi S, et al. Cryptococcal meningitis (C. neoformans var. gattii) leading to blindness in previously healthy Melanesian adults in Papua New Guinea. Q J Med. 1994;87:343–349. | |
Trachtenberg JD, Kambugu AD, McKellar M, et al. The medical management of central nervous system infections in Uganda and the potential impact of an algorithm-based approach to improve outcomes. Int J Infect Dis. 2007;11:524–530. | |
Moosa MY, Coovadia YM. Cryptococcal meningitis in Durban, South Africa: a comparison of clinical features, laboratory findings, and outcome for human immunodeficiency virus (HIV)-positive and HIV-negative patients. Clin Infect Dis. 1997;24:131–134. | |
Kabanda T, Siedner MJ, Klausner JD, Muzoora C, Boulware DR. Point-of-care diagnosis and prognostication of cryptococcal meningitis with the cryptococcal antigen lateral flow assay on cerebrospinal fluid. Clin Infect Dis. 2014;58:113–116. | |
Rugemalila J, Maro VP, Kapanda G, Ndaro AJ, Jarvis JN. Cryptococcal antigen prevalence in HIV-infected Tanzanians: a cross-sectional study and evaluation of a point-of-care lateral flow assay. Trop Med Int Health. 2013;18:1075–1079. | |
McMullan BJ, Halliday C, Sorrell TC, et al. Clinical utility of the cryptococcal antigen lateral flow assay in a diagnostic mycology laboratory. PLoS One. 2012;7:e49541. | |
Jarvis JN, Percival A, Bauman S, et al. Evaluation of a novel point-of-care cryptococcal antigen test on serum, plasma, and urine from patients with HIV-associated cryptococcal meningitis. Clin Infect Dis. 2011;53:1019–1023. | |
World Health Organization. Rapid Advice: Diagnosis, Prevention and Management of Cryptococcal Disease in HIV-Infected Adults, Adolescents and Children. Geneva: WHO; 2011. Available from: http://whqlibdoc.who.int/publications/2011/9789241502979_eng.pdf. Accessed February 13, 2014. | |
Brouwer AE, Rajanuwong A, Chierakul W, et al. Combination antifungal therapies for HIV-associated cryptococcal meningitis: a randomised trial. Lancet. 2004;363:1764–1767. | |
Bicanic T, Muzoora C, Brouwer AE, et al. Independent association between rate of clearance of infection and clinical outcome of HIV-associated cryptococcal meningitis: analysis of a combined cohort of 262 patients. Clin Infect Dis. 2009;49:702–709. | |
Andes D. Pharmacokinetics and pharmacodynamics of antifungals. Infect Dis Clin North Am. 2006;20:679–697. | |
Denning DW, Hope WW. Therapy for fungal diseases: opportunities and priorities. Trends Microbiol. 2010;18:195–204. | |
Cornely OA, Maertens J, Bresnik M, et al. Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial). Clin Infect Dis. 2007;44:1289–1297. | |
Hamill RJ, Sobel JD, El-Sadr W, et al. Comparison of 2 doses of liposomal amphotericin B and conventional amphotericin B deoxycholate for treatment of AIDS-associated acute cryptococcal meningitis: a randomized, double-blind clinical trial of efficacy and safety. Clin Infect Dis. 2010;51:225–232. | |
Leenders AC, Reiss P, Portegies P, et al. Liposomal amphotericin B (AmBisome) compared with amphotericin B both followed by oral fluconazole in the treatment of AIDS-associated cryptococcal meningitis. AIDS. 1997;11:1463–1471. | |
Chen SC. Cryptococcosis in Australasia and the treatment of cryptococcal and other fungal infections with liposomal amphotericin B. J Antimicrob Chemother. 2002;49 Suppl 1:57–61. | |
Bicanic T, Ogden D, Whitney L, Loyse A, Jarvis J. British HIV Association opportunistic infection guidelines: in defence of amphotericin B deoxycholate. HIV Med. 2012;13:636–637. | |
Pappas PG, Chetchotisakd P, Larsen RA, et al. A phase II randomized trial of amphotericin B alone or combined with fluconazole in the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2009;48:1775–1783. | |
Rajasingham R, Meya DB, Boulware DR. Integrating cryptococcal antigen screening and pre-emptive treatment into routine HIV care. J Acquir Immune Defic Syndr. 2012;59:e85–e91. | |
Jackson AT, Nussbaum JC, Phulusa J, et al. A phase II randomized controlled trial adding oral flucytosine to high-dose fluconazole, with short-course amphotericin B, for cryptococcal meningitis. AIDS. 2012;26:1363–1370. | |
Butler EK, Boulware DR, Bohjanen PR, Meya DB. Long term 5-year survival of persons with cryptococcal meningitis or asymptomatic subclinical antigenemia in Uganda. PLoS One. 2012;7:e51291. | |
Day JN, Chau TT, Lalloo DG. Combination antifungal therapy for cryptococcal meningitis. N Engl J Med. 2013;368:2522–2523. | |
Loyse A, Dromer F, Day J, Lortholary O, Harrison TS. Flucytosine and cryptococcosis: time to urgently address the worldwide accessibility of a 50-year-old antifungal. J Antimicrob Chemother. 2013;68:2435–2444. | |
O’Connor L, Livermore J, Sharp AD, et al. Pharmacodynamics of liposomal amphotericin B and flucytosine for cryptococcal meningoencephalitis: safe and effective regimens for immunocompromised patients. J Infect Dis. 2013;208:351–361. | |
Dromer F, Bernede-Bauduin C, Guillemot D, Lortholary O. Major role for amphotericin B-flucytosine combination in severe cryptococcosis. PLoS One. 2008;3:e2870. | |
Saag MS, Cloud GA, Graybill JR, et al. A comparison of itraconazole versus fluconazole as maintenance therapy for AIDS-associated cryptococcal meningitis. National Institute of Allergy and Infectious Diseases Mycoses Study Group. Clin Infect Dis. 1999;28:291–296. | |
Andes D, Pascual A, Marchetti O. Antifungal therapeutic drug monitoring: established and emerging indications. Antimicrob Agents Chemother. 2009;53:24–34. | |
Bicanic T, Wood R, Bekker LG, Darder M, Meintjes G, Harrison TS. Antiretroviral roll-out, antifungal roll-back: access to treatment for cryptococcal meningitis. Lancet Infect Dis. 2005;5:530–531. | |
Loyse A, Thangaraj H, Easterbrook P, et al. Cryptococcal meningitis: improving access to essential antifungal medicines in resource-poor countries. Lancet Infect Dis. 2013;13:629–637. | |
Muzoora CK, Kabanda T, Ortu G, et al. Short course amphotericin B with high dose fluconazole for HIV-associated cryptococcal meningitis. J Infect. 2012;64:76–81. | |
Loyse A, Wilson D, Meintjes G, et al. Comparison of the early fungicidal activity of high-dose fluconazole, voriconazole, and flucytosine as second-line drugs given in combination with amphotericin B for the treatment of HIV-associated cryptococcal meningitis. Clin Infect Dis. 2012;54:121–128. | |
Rajasingham R, Rolfes MA, Birkenkamp KE, Meya DB, Boulware DR. Cryptococcal meningitis treatment strategies in resource-limited settings: a cost-effectiveness analysis. PLoS Med. 2012;9:e1001316. | |
Mayanja-Kizza H, Oishi K, Mitarai S, et al. Combination therapy with fluconazole and flucytosine for cryptococcal meningitis in Ugandan patients with AIDS. Clin Infect Dis. 1998;26:1362–1366. | |
Schaars CF, Meintjes GA, Morroni C, Post FA, Maartens G. Outcome of AIDS-associated cryptococcal meningitis initially treated with 200 mg/day or 400 mg/day of fluconazole. BMC Infect Dis. 2006;6:118. | |
Longley N, Muzoora C, Taseera K, et al. Dose response effect of high-dose fluconazole for HIV-associated cryptococcal meningitis in southwestern Uganda. Clin Infect Dis. 2008;47:1556–1561. | |
Nussbaum JC, Jackson A, Namarika D, et al. Combination flucytosine and high-dose fluconazole compared with fluconazole monotherapy for the treatment of cryptococcal meningitis: a randomized trial in Malawi. Clin Infect Dis. 2010;50:338–344. | |
Sudan A, Livermore J, Howard SJ, et al. Pharmacokinetics and pharmacodynamics of fluconazole for cryptococcal meningoencephalitis: implications for antifungal therapy and in vitro susceptibility breakpoints. Antimicrob Agents Chemother. 2013;57:2793–2800. | |
Milefchik E, Leal MA, Haubrich R, et al. Fluconazole alone or combined with flucytosine for the treatment of AIDS-associated cryptococcal meningitis. Med Mycol. 2008;46:393–395. | |
St George’s University of London (UK). Advancing Cryptococcal meningitis Treatment for Africa: Oral fluconazole plus flucytosine or one week amphotericin B-based therapy vs two weeks amphotericin B-based therapy for initial treatment of HIV-associated cryptococcal meningitis. Available from: http://www.controlled-trials.com/ISRCTN45035509. ISRCTN identifier: ISRCTN45035509. Accessed February 28, 2014. | |
Bozzette SA, Larsen RA, Chiu J, et al. A placebo-controlled trial of maintenance therapy with fluconazole after treatment of cryptococcal meningitis in the acquired immunodeficiency syndrome. California Collaborative Treatment Group. N Engl J Med. 1991;324:580–584. | |
Powderly WG, Saag MS, Cloud GA, et al. A controlled trial of fluconazole or amphotericin B to prevent relapse of cryptococcal meningitis in patients with the acquired immunodeficiency syndrome. The NIAID AIDS Clinical Trials Group and Mycoses Study Group. N Engl J Med. 1992;326:793–798. | |
Collett G, Parrish A. Fluconazole donation and outcomes assessment in cryptococcal meningitis. S Afr Med J. 2007;97:175–176. | |
Jarvis JN, Meintjes G, Williams Z, Rebe K, Harrison TS. Symptomatic relapse of HIV-associated cryptococcal meningitis in South Africa: the role of inadequate secondary prophylaxis. S Afr Med J. 2010;100:378–382. | |
Mussini C, Pezzotti P, Miro JM, et al. Discontinuation of maintenance therapy for cryptococcal meningitis in patients with AIDS treated with highly active antiretroviral therapy: an international observational study. Clin Infect Dis. 2004;38:565–571. | |
Vibhagool A, Sungkanuparph S, Mootsikapun P, et al. Discontinuation of secondary prophylaxis for cryptococcal meningitis in human immunodeficiency virus-infected patients treated with highly active antiretroviral therapy: a prospective, multicenter, randomized study. Clin Infect Dis. 2003;36:1329–1331. | |
Martínez E, García-Viejo MA, Marcos MA, et al. Discontinuation of secondary prophylaxis for cryptococcal meningitis in HIV-infected patients responding to highly active antiretroviral therapy. AIDS. 2000;14:2615–2617. | |
Rollot F, Bossi P, Tubiana R, et al. Discontinuation of secondary prophylaxis against cryptococcosis in patients with AIDS receiving highly active antiretroviral therapy. AIDS. 2001;15:1448–1449. | |
Seddon J, Mangeya N, Miller RF, Corbett EL, Ferrand RA. Recurrence of cryptococcal meningitis in HIV-infected patients following immune reconstitution. Int J STD AIDS. 2009;20:274–275. | |
Singh N, Lortholary O, Alexander BD, et al. An immune reconstitution syndrome-like illness associated with Cryptococcus neoformans infection in organ transplant recipients. Clin Infect Dis. 2005;40:1756–1761. | |
Singh N, Perfect JR. Immune reconstitution syndrome associated with opportunistic mycoses. Lancet Infect Dis. 2007;7:395–401. | |
Singh N, Lortholary O, Alexander BD, et al. Antifungal management practices and evolution of infection in organ transplant recipients with Cryptococcus neoformans infection. Transplantation. 2005;80:1033–1039. | |
Morera-López Y, Torres-Rodríguez JM, Jiménez-Cabello T, Baró-Tomás T. Cryptococcus gattii: in vitro susceptibility to the new antifungal albaconazole versus fluconazole and voriconazole. Med Mycol. 2005;43:505–510. | |
Chong HS, Dagg R, Malik R, Chen S, Carter D. In vitro susceptibility of the yeast pathogen cryptococcus to fluconazole and other azoles varies with molecular genotype. J Clin Microbiol. 2010;48:4115–4120. | |
Smith RM, Nguyen TA, Ha HT, et al. Prevalence of cryptococcal antigenemia and cost-effectiveness of a cryptococcal antigen screening program – Vietnam. PLoS One. 2013;8:e62213. | |
Beyene T, Woldeamanuel Y, Asrat D, Ayana G, Boulware DR. Comparison of cryptococcal antigenemia between antiretroviral naive and antiretroviral experienced HIV positive patients at two hospitals in Ethiopia. PLoS One. 2013;8:e75585. | |
Alemu AS, Kempker RR, Tenna A, et al. High prevalence of cryptococcal antigenemia among HIV-infected patients receiving antiretroviral therapy in Ethiopia. PLoS One. 2013;8:e58377. | |
French N, Gray K, Watera C, et al. Cryptococcal infection in a cohort of HIV-1-infected Ugandan adults. AIDS. 2002;16:1031–1038. | |
Liechty CA, Solberg P, Were W, et al. Asymptomatic serum cryptococcal antigenemia and early mortality during antiretroviral therapy in rural Uganda. Trop Med Int Health. 2007;12:929–935. | |
Govender NP, Chetty V, Roy M, et al. Phased implementation of screening for cryptococcal disease in South Africa. S Afr Med J. 2012;102:914–917. | |
Jarvis JN, Harrison TS, Lawn SD, Meintjes G, Wood R, Cleary S. Cost effectiveness of cryptococcal antigen screening as a strategy to prevent HIV-associated cryptococcal meningitis in South Africa. PLoS One. 2013;8:e69288. | |
Jarvis JN, Lawn SD, Vogt M, Bangani N, Wood R, Harrison TS. Screening for cryptococcal antigenemia in patients accessing an antiretroviral treatment program in South Africa. Clin Infect Dis. 2009;48:856–862. | |
Meya DB, Manabe YC, Castelnuovo B, et al. Cost-effectiveness of serum cryptococcal antigen screening to prevent deaths among HIV-infected persons with a CD4+ cell count ≤100 cells/microL who start HIV therapy in resource-limited settings. Clin Infect Dis. 2010;51:448–455. | |
Jarvis JN, Govender N, Chiller T, et al. Cryptococcal antigen screening and preemptive therapy in patients initiating antiretroviral therapy in resource-limited settings: a proposed algorithm for clinical implementation. J Int Assoc Physicians AIDS Care (Chic). 2012;11:374–379. | |
Meyer AC, Kendi CK, Penner JA, et al. The impact of routine cryptococcal antigen screening on survival among HIV-infected individuals with advanced immunosuppression in Kenya. Trop Med Int Health. 2013;18:495–503. | |
Chang LW, Phipps WT, Kennedy GE, Rutherford GW. Antifungal interventions for the primary prevention of cryptococcal disease in adults with HIV. Cochrane Database Syst Rev. 2005:CD004773. | |
Parkes-Ratanshi R, Wakeham K, Levin J, et al. Primary prophylaxis of cryptococcal disease with fluconazole in HIV-positive Ugandan adults: a double-blind, randomised, placebo-controlled trial. Lancet Infect Dis. 2011;11:933–941. | |
Apisarnthanarak A, Mundy LM. The impact of primary prophylaxis for cryptococcosis on fluconazole resistance in Candida species. J Acquir Immune Defic Syndr. 2008;47:644–645. | |
Bicanic T, Brouwer AE, Meintjes G, et al. Relationship of cerebrospinal fluid pressure, fungal burden and outcome in patients with cryptococcal meningitis undergoing serial lumbar punctures. AIDS. 2009;23:701–706. | |
Graybill JR, Sobel J, Saag M, et al. Diagnosis and management of increased intracranial pressure in patients with AIDS and cryptococcal meningitis. The NIAID Mycoses Study Group and AIDS Cooperative Treatment Groups. Clin Infect Dis. 2000;30:47–54. | |
Pappas PG. Managing cryptococcal meningitis is about handling the pressure. Clin Infect Dis. 2005;40:480–482. | |
Dammert P, Bustamante B, Ticona E, et al. Treatment of cryptococcal meningitis in Peruvian AIDS patients using amphotericin B and fluconazole. J Infect. 2008;57:260–265. | |
de Vedia L, Arechavala A, Calderon MI, et al. Relevance of intracranial hypertension control in the management of Cryptococcus neoformans meningitis related to AIDS. Infection. 2013;41:1073–1077. | |
Wijewardana I, Jarvis JN, Meintjes G, Harrison TS, Bicanic T. Large volume lumbar punctures in cryptococcal meningitis clear cryptococcal antigen as well as lowering pressure. J Infect. 2011;63:484–486. | |
Manosuthi W, Sungkanuparph S, Chottanapund S, et al. Temporary external lumbar drainage for reducing elevated intracranial pressure in HIV-infected patients with cryptococcal meningitis. Int J STD AIDS. 2008;19:268–271. | |
Woodworth GF, McGirt MJ, Williams MA, Rigamonti D. The use of ventriculoperitoneal shunts for uncontrollable intracranial hypertension without ventriculomegally secondary to HIV-associated cryptococcal meningitis. Surg Neurol. 2005;63:529–531; discussion 531–532. | |
Newton PN, Thai le H, Tip NQ, et al. A randomized, double-blind, placebo-controlled trial of acetazolamide for the treatment of elevated intracranial pressure in cryptococcal meningitis. Clin Infect Dis. 2002;35:769–772. | |
Haddow LJ, Colebunders R, Meintjes G, et al. Cryptococcal immune reconstitution inflammatory syndrome in HIV-1-infected individuals: proposed clinical case definitions. Lancet Infect Dis. 2010;10:791–802. | |
Lawn SD, Harries AD, Anglaret X, Myer L, Wood R. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22:1897–1908. | |
Bisson GP, Nthobatsong R, Thakur R, et al. The use of HAART is associated with decreased risk of death during initial treatment of cryptococcal meningitis in adults in Botswana. J Acquir Immune Defic Syndr. 2008;49:227–229. | |
Klotz SA, Aziz Mohammed A, Girmai Woldemichael M, Worku Mitku M, Handrich M. Immune reconstitution inflammatory syndrome in a resource-poor setting. J Int Assoc Physicians AIDS Care (Chic). 2009;8:122–127. | |
Lawn SD, Bekker LG, Myer L, Orrell C, Wood R. Cryptococcocal immune reconstitution disease: a major cause of early mortality in a South African antiretroviral programme. AIDS. 2005;19:2050–2052. | |
Murdoch DM, Venter WD, Feldman C, Van Rie A. Incidence and risk factors for the immune reconstitution inflammatory syndrome in HIV patients in South Africa: a prospective study. AIDS. 2008;22:601–610. | |
French MA. HIV/AIDS: immune reconstitution inflammatory syndrome: a reappraisal. Clin Infect Dis. 2009;48:101–107. | |
Longley N, Harrison TS, Jarvis JN. Cryptococcal immune reconstitution inflammatory syndrome. Curr Opin Infect Dis. 2013;26:26–34. | |
Lortholary O, Fontanet A, Memain N, Martin A, Sitbon K, Dromer F. Incidence and risk factors of immune reconstitution inflammatory syndrome complicating HIV-associated cryptococcosis in France. AIDS. 2005;19:1043–1049. | |
Bicanic T, Meintjes G, Rebe K, et al. Immune reconstitution inflammatory syndrome in HIV-associated cryptococcal meningitis: a prospective study. J Acquir Immune Defic Syndr. 2009;51:130–134. | |
Lesho E. Evidence base for using corticosteroids to treat HIV-associated immune reconstitution syndrome. Expert Rev Anti Infect Ther. 2006;4:469–478. | |
Chang C, Dorasamay A, Elliott J, et al. HIV+ patients with CM who attain CSF sterility pre-cART commencement experience improved outcomes in the first 24 weeks. Poster presented at: 19th Conference on Retroviruses and Opportunistic Infections; March 5–8, 2012; Seattle, WA. | |
Jackson A, van der Horst C. New insights in the prevention, diagnosis, and treatment of cryptococcal meningitis. Curr HIV/AIDS Rep. 2012;9:267–277. | |
Manosuthi W, Chottanapund S, Sungkanuparph S. Mortality rate of early versus deferred initiation of antiretroviral therapy in HIV-1-infected patients with cryptococcal meningitis. J Acquir Immune Defic Syndr. 2008;48:508–509. | |
Zolopa A, Andersen J, Powderly W, et al. Early antiretroviral therapy reduces AIDS progression/death in individuals with acute opportunistic infections: a multicenter randomized strategy trial. PLoS One. 2009;4:e5575. | |
Bisson GP, Molefi M, Bellamy S, et al. Early versus delayed antiretroviral therapy and cerebrospinal fluid fungal clearance in adults with HIV and cryptococcal meningitis. Clin Infect Dis. 2013;56:1165–1173. | |
Makadzange AT, Ndhlovu CE, Takarinda K, et al. Early versus delayed initiation of antiretroviral therapy for concurrent HIV infection and cryptococcal meningitis in sub-Saharan Africa. Clin Infect Dis. 2010;50:1532–1538. | |
Boulware D, Meya D, Muzoora C, et al. ART initiation within the first 2 weeks of cryptococcal meningitis is associated with higher mortality: a multisite randomized trial. Poster presented at: 20th Conference on Retroviruses and Opportunistic Infections; March 3–6, 2013; Atlanta, GA. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.




