Back to Journals » OncoTargets and Therapy » Volume 7
Conventional fractionated helical tomotherapy for patients with small to medium hepatocellular carcinomas without portal vein tumor thrombosis
Authors Jung J, Kong M , Hong SE
Received 18 June 2014
Accepted for publication 24 July 2014
Published 26 September 2014 Volume 2014:7 Pages 1769—1775
DOI https://doi.org/10.2147/OTT.S69618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Faris Farassati
Jinhong Jung, Moonkyoo Kong, Seong Eon Hong
Department of Radiation Oncology, Kyung Hee University Medical Center, Kyung Hee University School of Medicine, Seoul, Republic of Korea
Background: The purpose of this study was to evaluate clinical outcomes of conventional fractionated helical tomotherapy in patients with small to medium hepatocellular carcinomas (HCCs) without portal vein tumor thrombosis.
Methods: Patients with up to four HCC lesions not treatable by surgery or percutaneous ablative therapies, <10 cm in the longest diameter, and no evidence of major vascular invasion were included. From January 2008 to January 2013, 20 patients with 33 tumors met the eligibility criteria and received definitive or salvage helical tomotherapy. The most commonly prescribed dose fractionation schedule was a total dose of 50 Gy with a daily dose of 2.5 Gy. Treatment response, survival, and radiation-induced toxicities were retrospectively reviewed.
Results: The median follow-up period after radiotherapy for all patients was 24.9 (range 7.8–79.2) months. Objective responses (complete response or partial response) occurred in 30 of 33 lesions (90.9%). Eight (24.2%) lesions showed local recurrence and the actuarial local control rate at 2 years was 69.5%. Intrahepatic recurrence-free survival and overall survival rates at 2 years were 45.7% and 71.1%, respectively. Age, Child–Pugh class, tumor response, local recurrence status, and intrahepatic recurrence status were significantly associated with overall survival on univariate analysis. Among these parameters, only local recurrence status showed marginal statistical significance on multivariate analysis (P=0.068). The overall survival rate at 2 years was 50% for patients who experienced local recurrence, but 87.5% for those who did not. No patient experienced grade 2 or greater general or gastrointestinal toxicity. There were no cases of radiation-induced liver disease.
Conclusion: Conventional fractionated helical tomotherapy for patients with less than four small to medium HCCs without portal vein tumor thrombosis yielded favorable local control and overall survival without severe complications.
Keywords: hepatocellular carcinoma, conventional fractionated radiotherapy, helical tomotherapy
Introduction
Advances in our understanding of partial liver tolerance of radiotherapy (RT), diagnostic imaging, RT planning, techniques to account for respiratory motion of the liver, techniques to target the liver tumor that use image-guided RT, and the increasing availability of stereotactic RT and charged particle therapy have permitted us to escalate RT doses to focal hepatocellular carcinoma (HCC) without dose-limiting toxicity.1 Furthermore, several studies that used three-dimensional conformal radiotherapy (3D-CRT) at a higher dose than conventional RT suggested that HCC is a radiosensitive tumor.2–8 These efforts have led to a resurgence of interest in curative treatment of HCC using RT.
However, previous studies that performed conventional fractionated RT included cohorts heterogeneous in terms of clinical conditions, ie, tumor size, presence of vascular invasion, underlying liver function, and number of tumors.2–4,6–13 In addition, the intent of RT with or without other modalities included both salvage and palliation. On the other hand, several studies have reported encouraging treatment outcomes for patients with early or intermediate HCC treated with stereotactic body radiation therapy (SBRT).14–18 However, hypofractionated RT was performed for patients with HCC in those studies. Therefore, it remains difficult to determine the true outcome of conventional fractionated RT for early and intermediate HCC. Furthermore, studies examining high-dose irradiation using conventional fractionated helical tomotherapy are scarce.
The purpose of this study was to evaluate clinical outcomes of conventional fractionated helical tomotherapy for patients with less than four small to medium HCCs without portal vein tumor thrombosis (PVTT).
Materials and methods
Patient selection
The records of 50 patients with HCC who received RT and were registered in an institutional database were retrospectively reviewed. Eligibility criteria were as follows: HCC confirmed by clinical examination or histology; HCC not treatable by surgery or percutaneous ablative therapies; an incomplete response after transcatheter arterial chemoembolization or unsuitable for this procedure; receipt of helical tomotherapy with definitive or salvage intent; HCC <10 cm in the longest diameter, the presence of up to four lesions, and confined to the liver; HCC with no evidence of major vascular invasion; no extrahepatic metastases; good general condition with Eastern Cooperative Oncology Group (ECOG) performance status ≤2; and Child–Pugh A or B liver function. Among the 50 reviewed patients, 20 patients with 33 tumors met the eligibility criteria and were included in this study. A diagnosis of HCC was based on the practice guidelines developed by the Korean Liver Cancer Study Group.19 Cancer stage for each patient was assigned based on the American Joint Committee on Cancer (AJCC) staging system (7th edition). All research was carried out in compliance with the Declaration of Helsinki.
RT procedure
All patients underwent computed tomography (CT) simulation in the supine position after immobilization with a posterior vacuum bag and an anterior vacuum-sealed cover sheet (BodyFix, Medical Intelligence Medizintechnik GmBH, Schwabmünchen, Germany). Contrast enhanced CT images were acquired with 3 mm slice thickness during free breathing, and all patients were asked to take shallow breaths to reduce movement of the liver by respiration. The simulation CT data were transferred to a Hi · Art Planning Station (TomoTherapy Inc., Madison, WI, USA) for inverse planning. Gross tumor volume was delineated based on the visible gross tumor as seen on the CT and/or magnetic resonance image. Subsequently, a 5 mm margin was added to create the clinical target volume, and the planning target volume (PTV) margin was 10–15 mm from the clinical target volume, taking into account target movement associated with respiration. A dose of 2–4 Gy per fraction was given over 5 consecutive days per week to a total dose of 40–60 Gy according to the physician’s judgment with consideration of the patient’s general condition, PTV, and radiation dose delivered to normal liver. The most commonly prescribed dose fractionation schedule was a total dose of 50 Gy with a daily dose of 2.5 Gy.
Each treatment plan was evaluated using a dose-volume histogram and visually inspecting isodose curves. In general, we considered plans acceptable if the PTV was covered by 95% of the isodose curve, which was normalized to the center of the PTV; inhomogeneity of the PTV ranged from 95% to 107%, and doses to normal structures were limited in their tolerances. The dose constraints for normal liver were that no more than 30% of a normal liver could receive more than 27 Gy (V27 <30%) and no more than 50% of a normal liver could receive more than 24 Gy (V24 <50%). Additionally, the mean normal liver dose needed to be less than 28 Gy. RT was performed using a TomoTherapy device (TomoTherapy Inc.). Triangulation marks were used to ensure that the patient did not roll and to be able to quickly position the patient in the correct location. Image guidance, including 3.5-mega voltage fan beam CT imaging, was performed prior to administration of each RT fraction using a CT detector mounted on a ring gantry.
Follow-up
All patients were examined at least once per week during their RT course to assess for acute toxicity. After treatment, the patients were followed up every 1–3 months. Follow-up consisted of physical examinations, complete blood counts, biochemical profiles, tumor markers, and dynamic CT or magnetic resonance image studies. Treatment response was determined according to the modified Response Evaluation Criteria in Solid Tumors.20 A complete response was defined as the disappearance of any intratumoral arterial enhancement in all target lesions; a partial response was defined as at least a 30% decrease in the sum of the diameters of the viable (enhancement in the arterial phase) target lesions; progressive disease was defined as a ≥20% increase in the sum of the diameters of viable (enhancing) target lesions or the appearance of any new malignant lesions; and stable disease was defined as a tumor response between partial response and progressive disease. To fully evaluate the true response of the tumor after RT, we assessed the treatment response when the enhanced lesion was no longer shrinking in size. An objective response rate was defined as the sum of the complete response and partial response rates. The appearance of a new enhanced lesion or progression within the PTV was defined as a local recurrence; the new intrahepatic appearance of tumor outside the PTV was defined as an intrahepatic recurrence; and any recurrence outside the liver was defined as a distant metastasis. The lesions that showed local recurrence received further treatments; however, the lesions that showed an objective response without local recurrence or stable disease did not. The alpha-fetoprotein (AFP) level was calculated by calculating the post-RT AFP level/pre-RT AFP level, and AFP response was defined as an AFP level change <1. Radiation-induced general and gastrointestinal toxicities were assessed using the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0. Patients who had baseline symptoms were scored based on CTCAE toxicity grade both before and after RT, and the difference in grade was recorded. Radiation-induced liver disease and radiation-induced hepatitis B virus reactivation were also evaluated and the detailed definitions are given in our previous report.21
Statistical analysis
Cumulative survival was determined using the Kaplan–Meier method and the survival differences were analyzed by the log-rank test. The time to local recurrence, intrahepatic recurrence, distant metastasis, and overall survival were calculated from the date of RT completion. Multivariate analyses was performed to assess relationships between cumulative survival and possible prognostic variables using the Cox proportional hazards model and included only those variables with a P-value <0.05 as determined in the univariate analysis. All statistical analyses were performed using Statistical Package for the Social Sciences version 18.0 software (SPSS Inc., Chicago, IL, USA).
Results
Patient characteristics are summarized in Table 1. Nine (45.0%) patients were ECOG 1 and two (10.0%) were ECOG 2. Fourteen (70.0%) patients had received other treatments before RT. Twelve (60.0%) patients were treated with transcatheter arterial chemoembolization and two (10.0%) patients were treated with transcatheter arterial chemoembolization and surgical resection. Eleven (33.3%) lesions were treated with a total dose of 50 Gy in 2.5 Gy-fraction, six (18.2%) with 60 Gy in 3 Gy-fraction, four (12.1%) with 55 Gy in 2.2 Gy-fraction, and the remaining lesions (36.4%) were treated with a total dose ranging from 40 to 59.4 Gy in 10–28 fractions.
A complete response was noted in 23 of 33 lesions (69.7%), a partial response in seven (21.2%), stable disease in one (3.0%), and progressive disease in two (6.1%). An objective response (complete response or partial response) occurred in 30 lesions (90.9%), and 17 patients (85.0%). The median follow-up period after RT for all patients was 24.9 (range 7.8–79.2) months. Among the 33 lesions, eight (24.2%) showed local recurrence and the actuarial local control rates at one and 2 years were 81.6% and 69.5%, respectively (Figure 1). Intrahepatic recurrence-free survival and overall survival rates were 65.0% and 90.0% at one year and 45.7% and 71.1% at 2 years, respectively (Figure 2). Intrahepatic recurrence occurred in 12 (60.0%) patients, and eleven (55.0%) died during the follow-up period. Distant metastasis-free survival rates at one and 2 years were 90.0% and 80.0%, respectively. Four (20.0%) patients experienced distant metastasis and the sites of distant metastasis were lungs in two, both lungs and adrenal glands in one, and bone in one patient.
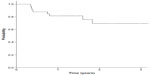  | Figure 1 Local control rates at 1 and 2 years were 81.6% and 69.5%, respectively. |
  | Figure 2 Intrahepatic recurrence-free survival and overall survival rates were 65.0% and 90.0% at 1 year, and 45.7% and 71.1% at 2 years, respectively. |
No significant prognostic factor for local recurrence or intrahepatic recurrence was noted on univariate analysis. Age, Child–Pugh class, tumor response (complete response versus partial response + stable disease + progressive disease), local recurrence status, and intrahepatic recurrence status were significantly associated with overall survival (Table 2). Among these parameters, only local recurrence status showed marginal statistical significance (P=0.068; hazard ratio 9.326; 95% confidence interval 0.848–102.532) on multivariate analysis. The overall survival rate at 2 years was 50% for patients who experienced local recurrence, but was 87.5% for those who did not.
All patients received a complete course of scheduled RT without treatment interruption. No patient experienced grade 2 or greater general or gastrointestinal toxicity. Grade 1 toxicity developed in 16 (80.0%) patients. Ten (50.0%) patients experienced grade 1 general toxicity in the form of fatigue, and nine (45.0%) patients experienced grade 1 gastrointestinal toxicity, which included four with nausea, three with gastritis, and two with dyspepsia, but all recovered spontaneously. Two (10.0%) patients experienced radiation-induced hepatitis B virus reactivation. There was no case of radiation-induced liver disease.
Discussion
The present study evaluated patients who had up to four small-sized to medium-sized (<10 cm) HCC lesions treated with conventional fractionated intensity-modulated radiotherapy (IMRT). None of the patients had PVTT and they were classified as stage I–IIIA using the AJCC staging system. Because there was variation in the total dose and in the fraction dose, we used the biologically effective dose (BED) for analysis, and all patients received IMRT with a median RT dose of 67.1 Gy10 BED. The results of the present study revealed one-year and 2-year actuarial local control rates of 81.6% and 69.5%, respectively, and one-year and 2-year overall survival rates of 90.0% and 71.1%, respectively. Although caution must be taken in interpreting clinical outcomes due to the heterogeneity of patient characteristics, these outcomes were more favorable compared with those of previous studies, which showed one-year and 2-year local control rates ranging from 77.9% to 100% and 61.1% to 93%, respectively, and one-year and 2-year overall survival rates ranging from 41.8% to 72.0% and 19.9% to 69.1%, respectively.3,4,6–8,11,12,21,22 We speculated that there were several reasons for our superior results. First of all, we included patients with small-sized to medium-sized tumors (median 1.6 cm) without PVTT, which were shown to be better prognostic conditions in terms of local control and overall survival in previous studies.3,10,21,23–25 Nearly all other studies reporting treatment outcomes of conventional fractionated 3D-CRT included larger-sized tumors (median tumor size range of 3.2–10 cm) and a high proportion of patients with PVTT (range 0%–100%).2–4,6–8,10,11,13 Second, we utilized relatively high doses of irradiation (median 67.1 Gy10), using IMRT without serious complications. RT dose is another important prognostic factor not only for local control, but also overall survival.2,3,6,10 The RT dose in this study was higher than the median RT dose (53.1 Gy10) of 3D-CRT used for HCC in Korea and those used in previous studies (range of 43.1–65.9 Gy).6,8,10,13,21
The tumor response after RT in HCC patients is a frequently used end point. In order to fully evaluate the true response of the tumor, the tumor response was evaluated when the enhanced lesion was no longer shrinking in size under continuous observation in this study. However, the evaluation time and the evaluation tools for treatment response following RT varied significantly in previous studies, and treatment response could vary depending on the duration of follow-up after RT.2–4,6–8,11,13,21–23 There is little consensus regarding the optimal time for treatment response assessment after RT in patients with HCC. We are unsure at this time whether the improved tumor response with dose escalation could be correlated with improved survival. Although some studies demonstrated the importance of tumor response as a prognostic factor for local control or overall survival,6,8,13 most of the studies mentioned above did not identify a relationship between tumor response and oncological outcomes.2–4,7,11,21–23 In this study, tumor response (complete response versus partial response + stable disease + progressive disease) was not significantly associated with local control. Furthermore, Child–Pugh class, tumor response, local recurrence status, and intrahepatic recurrence status were significantly associated with overall survival on univariate analysis, but only local recurrence status showed marginal statistical significance on multivariate analysis. Kim et al demonstrated that patients with HCC and high standardized uptake values (SUV) obtained from positron emission tomography with fluorine-18-fluorodeoxyglucose using a cutoff of 2.5 showed higher response rates than those with low SUV after RT, but this did not result in a survival benefit.26 They hypothesized that because rapidly proliferating tumors require increased glucose metabolism, the SUV ratio may reflect the tumor volume doubling time. Rapidly proliferating tumors tend to have more aggressive biological behavior and also are more radiosensitive. These characteristics may have translated into a favorable response to radiotherapy in the high-SUV ratio group. Thus, care must be taken when interpreting tumor response as a surrogate for local control or overall survival, and further studies determining the optimum time needed for evaluation of response should be conducted.
SBRT is one of the fastest growing alternative modalities for unresectable HCC. SBRT showed encouraging treatment outcomes, with one-year local control and overall survival rates of 65%–100% and 48%–93%, respectively.14–18 However, those studies had strict inclusion criteria, ie, an HCC size <6–7 cm, ≤3 lesions, and sufficient distance (>0.5–2 cm) between the HCC and adjacent organs at risk, such as the duodenum, stomach, colon, and spinal cord. The local control rate of 81.6% and overall survival rate of 90% at one year in the present study is encouraging considering the relatively unfavorable characteristics of our patient cohort, including HCC size <10 cm and ≤4 lesions, when compared with those used in the SBRT studies. Radiofrequency ablation for HCC showed 2-year local control of 82%–98%.27–29 However, Livraghi et al demonstrated that radiofrequency ablation achieved 90% of complete necrosis in HCC <3 cm, but 71% in medium (3–5 cm) and 45% in large (5.1–9 cm) HCC.28 Although additional studies with larger sample size and longer follow-up are required to confirm the favorable results of our study, we believe that conventional fractionated IMRT could be a good treatment option for HCC patients who are unfit for SBRT or radiofrequency ablation.
The present study has limitations in terms of its retrospective design, which has inherent weaknesses including selection bias, a small number of patients, and short follow-up period. Nevertheless, it has unique strengths in that we utilized a homogeneous study cohort with limited numbers of small-sized to medium-sized HCCs and a uniform IMRT technique. In addition, to the best of our knowledge, this is the first report of clinical outcomes of definitive or salvage helical tomotherapy for HCC without PVTT.
In conclusion, conventional fractionated helical tomotherapy for patients with less than four small to medium HCCs without PVTT yielded favorable local control and overall survival without severe complications.
Author contributions
All authors made substantive contributions to the article and assume full responsibility for its content. Also, all authors fulfilled the International Committee of Medical Journal Editors requirements for authorship.
Disclosure
The authors report no conflicts of interest in this work.
References
Krishnan S, Dawson LA, Seong J, et al. Radiotherapy for hepatocellular carcinoma: an overview. Ann Surg Oncol. 2008;15(4):1015–1024. | |
Dawson LA, McGinn CJ, Normolle D, et al. Escalated focal liver radiation and concurrent hepatic artery fluorodeoxyuridine for unresectable intrahepatic malignancies. J Clin Oncol. 2000;18(11):2210–2218. | |
Seong J, Park HC, Han KH, Chon CY. Clinical results and prognostic factors in radiotherapy for unresectable hepatocellular carcinoma: a retrospective study of 158 patients. Int J Radiat Oncol Biol Phys. 2003;55(2):329–336. | |
Park HC, Seong J, Han KH, Chon CY, Moon YM, Suh CO. Dose-response relationship in local radiotherapy for hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2002;54(1):150–155. | |
Robertson JM, Lawrence TS, Dworzanin LM, et al. Treatment of primary hepatobiliary cancers with conformal radiation therapy and regional chemotherapy. J Clin Oncol. 1993;11(7):1286–1293. | |
Park W, Lim DH, Paik SW, et al. Local radiotherapy for patients with unresectable hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2005;61(4):1143–1150. | |
Mornex F, Girard N, Beziat C, et al. Feasibility and efficacy of high-dose three-dimensional-conformal radiotherapy in cirrhotic patients with small-size hepatocellular carcinoma non-eligible for curative therapies – mature results of the French Phase II RTF-1 trial. Int J Radiat Oncol Biol Phys. 2006;66(4):1152–1158. | |
Yoon SM, Lim YS, Won HJ, et al. Radiotherapy plus transarterial chemoembolization for hepatocellular carcinoma invading the portal vein: long-term patient outcomes. Int J Radiat Oncol Biol Phys. 2012;82(5):2004–2011. | |
Liang SX, Zhu XD, Lu HJ, et al. Hypofractionated three-dimensional conformal radiation therapy for primary liver carcinoma. Cancer. 2005;103(10):2181–2188. | |
Seong J, Lee IJ, Shim SJ, et al. A multicenter retrospective cohort study of practice patterns and clinical outcome on radiotherapy for hepatocellular carcinoma in Korea. Liver Int. 2009;29(2):147–152. | |
Liu MT, Li SH, Chu TC, et al. Three-dimensional conformal radiation therapy for unresectable hepatocellular carcinoma patients who had failed with or were unsuited for transcatheter arterial chemoembolization. Jpn J Clin Oncol. 2004;34(9):532–539. | |
Ben-Josef E, Normolle D, Ensminger WD, et al. Phase II trial of high-dose conformal radiation therapy with concurrent hepatic artery floxuridine for unresectable intrahepatic malignancies. J Clin Oncol. 2005;23(34):8739–8747. | |
Kim TH, Kim DY, Park JW, et al. Three-dimensional conformal radiotherapy of unresectable hepatocellular carcinoma patients for whom transcatheter arterial chemoembolization was ineffective or unsuitable. Am J Clin Oncol. 2006;29(6):568–575. | |
Mendez Romero A, Wunderink W, Hussain SM, et al. Stereotactic body radiation therapy for primary and metastatic liver tumors: a single institution phase I–II study. Acta Oncol. 2006;45(7):831–837. | |
Tse RV, Hawkins M, Lockwood G, et al. Phase I study of individualized stereotactic body radiotherapy for hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol. 2008;26(4):657–664. | |
Kwon JH, Bae SH, Kim JY, et al. Long-term effect of stereotactic body radiation therapy for primary hepatocellular carcinoma ineligible for local ablation therapy or surgical resection. Stereotactic radiotherapy for liver cancer. BMC Cancer. 2010;10:475. | |
Andolino DL, Johnson CS, Maluccio M, et al. Stereotactic body radiotherapy for primary hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2011;81(4):e447–e453. | |
Yoon SM, Lim YS, Park MJ, et al. Stereotactic body radiation therapy as an alternative treatment for small hepatocellular carcinoma. PLoS One. 2013;8(11):e79854. | |
Korean Liver Cancer Study Group and National Cancer Center, Korea. [Practice guidelines for management of hepatocellular carcinoma 2009]. Korean J Hepatol. 2009;15(3):391–423. Korean. | |
Lencioni R, Llovet JM. Modified RECIST (mRECIST) assessment for hepatocellular carcinoma. Semin Liver Dis. 2010;30(1):52–60. | |
Kong M, Hong SE, Choi WS, Choi J, Kim Y. Treatment outcomes of helical intensity-modulated radiotherapy for unresectable hepatocellular carcinoma. Gut Liver. 2013;7(3):343–351. | |
Ren ZG, Zhao JD, Gu K, et al. Three-dimensional conformal radiation therapy and intensity-modulated radiation therapy combined with transcatheter arterial chemoembolization for locally advanced hepatocellular carcinoma: an irradiation dose escalation study. Int J Radiat Oncol Biol Phys. 2011;79(2):496–502. | |
Kim SW, Oh D, Park HC, et al. Transcatheter arterial chemoembolization and radiation therapy for treatment-naïve patients with locally advanced hepatocellular carcinoma. Radiat Oncol J. 2014;32(1):14–22. | |
Zhou ZH, Liu LM, Chen WW, et al. Combined therapy of transcatheter arterial chemoembolisation and three-dimensional conformal radiotherapy for hepatocellular carcinoma. Br J Radiol. 2007;80(951):194–201. | |
Kang MK, Kim MS, Kim SK, et al. High-dose radiotherapy with intensity-modulated radiation therapy for advanced hepatocellular carcinoma. Tumori. 2012;97(6):724–731. | |
Kim JW, Seong J, Yun M, et al. Usefulness of positron emission tomography with fluorine-18-fluorodeoxyglucose in predicting treatment response in unresectable hepatocellular carcinoma patients treated with external beam radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82(3):1172–1178. | |
Lencioni RA, Allgaier HP, Cioni D, et al. Small hepatocellular carcinoma in cirrhosis: randomized comparison of radio-frequency thermal ablation versus percutaneous ethanol injection. Radiology. 2003;228(1):235–240. | |
Livraghi T, Lazzaroni S, Meloni F. Radiofrequency thermal ablation of hepatocellular carcinoma. Eur J Ultrasound. 2001;13(2):159–166. | |
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Radiofrequency ablation improves prognosis compared with ethanol injection for hepatocellular carcinoma ≤4 cm. Gastroenterology. 2004;127(6):1714–1723. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


