Back to Journals » Open Access Journal of Sports Medicine » Volume 6
Complications following arthroscopic fixation of acromioclavicular separations: a systematic review of the literature
Authors Woodmass J, Esposito J, Ono Y, Nelson A, Boorman R, Thornton G, Lo I
Received 25 August 2014
Accepted for publication 11 October 2014
Published 10 April 2015 Volume 2015:6 Pages 97—107
DOI https://doi.org/10.2147/OAJSM.S73211
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Freddie H Fu
Jarret M Woodmass,1 John G Esposito,1 Yohei Ono,1,2 Atiba A Nelson,1 Richard S Boorman,1 Gail M Thornton,1,3 Ian KY Lo1
1Department of Surgery, Section of Orthopaedic Surgery, McCaig Institute for Bone and Joint Health, University of Calgary, Calgary, AB, Canada; 2Department of Orthopaedic Surgery, Nagoya University Graduate School of Medicine, Nagoya, Japan; 3Department of Orthopaedics, University of British Columbia, Vancouver, BC, Canada
Purpose: Over the past decade, a number of arthroscopic or arthroscopically assisted reconstruction techniques have emerged for the management of acromioclavicular (AC) separations. These techniques provide the advantage of superior visualization of the base of the coracoid, less soft tissue dissection, and smaller incisions. While these techniques have been reported to provide excellent functional results with minimal complications, discrepancies exist within the literature. This systematic review aims to assess the rate of complications following these procedures.
Methods: Two independent reviewers completed a search of Medline, Embase, PubMed, and the Cochrane Library entries up to December 2013. The terms “Acromioclavicular Joint (MeSH)” OR “acromioclavicular* (text)” OR “coracoclavicular* (text)” AND “Arthroscopy (MeSH)” OR “Arthroscop* (text)” were used. Pooled estimates and 95% confidence intervals were calculated assuming a random-effects model. Statistical heterogeneity was quantified using the I2 statistic.
Level of evidence: IV
Results: A total of 972 abstracts met the search criteria. After removal of duplicates and assessment of inclusion/exclusion criteria, 12 articles were selected for data extraction. The rate of superficial infection was 3.8% and residual shoulder/AC pain or hardware irritation occurred at a rate of 26.7%. The rate of coracoid/clavicle fracture was 5.3% and occurred most commonly with techniques utilizing bony tunnels. Loss of AC joint reduction occurred in 26.8% of patients.
Conclusion: Arthroscopic AC reconstruction techniques carry a distinct complication profile. The TightRope/Endobutton techniques, when performed acutely, provide good radiographic outcomes at the expense of hardware irritation. In contrast, graft reconstructions in patients with chronic AC separations demonstrated a high risk for loss of reduction. Fractures of the coracoid/clavicle remain a significant complication occurring predominately with techniques utilizing bony tunnels.
Keywords: fracture, reduction, hardware irritation
Introduction
Acromioclavicular (AC) joint (ACJ) separations are common injuries that can result from sports activities and direct impact to the lateral aspect of the shoulder.1 ACJ separations were formally classified in 1963 by Tossy et al2 as types I through III based on pathology of the AC and coracoclavicular (CC) ligaments: I= AC sprain; II= AC tear/CC sprain; III= AC/CC tears. This was expanded by Rockwood and Green to the types I through VI Rockwood Classification.3 Most authors agree that type I and II injuries can be treated nonoperatively with satisfactory results,4,5 types IV–VI are best treated surgically, and there is continued debate regarding the most appropriate treatment for type III injuries.6–8
More than 60 different operative techniques have been described for the treatment of ACJ separations. 9–11 Currently, no single technique has gained widespread acceptance. This, in part, is related to the diversity of outcomes and the fact that each operative technique carries its own inherent complication profile. A recent review by Geaney et al12 assessed common mechanisms for failure of ACJ reconstructions and treatment options. These failures included hardware migration, persistent pain, distal clavicle osteolysis, clavicle fracture, coracoid fracture, graft failure, and/or recurrent separations.12
With the advent of arthroscopy, a number of newer arthroscopic or arthroscopically assisted techniques have emerged over the past decade.13–16 These techniques provide the advantage of superior visualization of the base of the coracoid, less soft tissue dissection, and smaller incisions.17 Additionally, these techniques have the theoretical benefit of allowing the surgeon to identify and treat associated injuries within the glenohumeral joint and subacromial space.9
While published articles using these techniques have reported excellent functional results9 with minimal complications,18 significant discrepancies also exist within the literature. For example, DeBerardino et al reported 100% good to excellent outcomes, with full return to preinjury level of activity at 6-months follow-up with no reports of complications (infection, hardware or graft failure) or loss of the interoperative reduction using the GraftRope technique.18 In contrast, Cook et al reported an 80% rate of loss of reduction with 88% resulting from hardware failure using a similar technique.10 Furthermore, there have been multiple reports of significant complication rates using arthroscopic or arthroscopically assisted techniques including: hardware erosion into the clavicle in over 40% of cases;19 hardware failures in 70% of cases;10 and, less commonly, persistent pain, infection, clavicle or coracoid fracture, CC calcification, and shoulder stiffness.20,21
This systematic review of literature aims to assess the complication rate following arthroscopic or arthroscopically assisted reconstruction of ACJ separations. Our goal was to determine the overall safety of arthroscopic ACJ reconstruction. We hypothesized that arthroscopic ACJ reconstruction would be a relatively safe technique with minimal complications.
Methods
All Level I–IV evidence in the English language was considered. Two independent reviewers completed a search of Medline, Embase, PubMed, and the Cochrane Library entries up to December 2013. The terms “Acromioclavicular Joint (MeSH)” OR “acromioclavicular* (text)” OR “coracoclavicular* (text)” AND “Arthroscopy (MeSH)” OR “Arthroscop* (text)” were used. Studies were included in this systematic review if they met the following criteria: 1) ACJ separation – types III, IV, or V as defined by Rockwood3 or an equivalent description; 2) arthroscopic or arthroscopically assisted fixation technique; 3) postoperative radiographic outcomes; 4) detailed description of patient demographics and postoperative complications (ie, the description of “no complications” was not sufficient for inclusion in this study – complications were only recorded if they were specifically mentioned); 5) greater than or equal to ten ACJ separations treated; and (6) English language.
Exclusion criteria included: 1) revision ACJ reconstruction studies; 2) skeletally immature patients; 3) polytrauma patients; 4) previous trauma/infection; 5) abstract-only entries; 6) case reports; 7) technical notes; 8) review articles; and 9) articles later updated with longer-term follow-up and a larger cohort. The references from the included studies and reviews were assessed for eligibility. All articles selected by both reviewers were included; discrepancies were assessed by the senior author to determine eligibility.
Data abstraction
Data from each study that met the inclusion criteria was extracted independently and then verified by the two reviewers. Both acute and chronic separations were included. An acute separation was defined as having undergone surgery within 3 weeks from the time of injury.
Data included: 1) number of patients; 2) number of ACJ reconstructions; 3) number of males and females; 4) patient age; 5) grade of ACJ separation according to Rockwood et al;3 6) duration of symptoms; 7) duration of follow-up; 8) type of reconstruction; 9) functional outcomes; and 10) complications. All complications were recorded including persistent pain, hardware irritation, infection, CC calcification, fracture, and the rate of subluxation/ dislocation.
Only radiographs were considered to be sufficient for documentation of the maintenance of anatomic reduction, a subluxation, or a dislocation. A dislocation was defined as 100% displacement of the ACJ or the description of complete loss of reduction. Subluxation was defined as a partial loss of reduction. Arthroscopic reconstructions were divided into anatomic and nonanatomic reconstructions. Anatomic reconstructions were those that attempted to reconstruct both the conoid and trapezoid ligaments, while all others were considered nonanatomic.
Statistics
Data were imported into StatsDirect statistical software and pooled estimates for rate of infection, fracture, loss of reduction, and CC calcification were calculated. Pooled estimates and 95% confidence intervals (CI) were calculated assuming a random-effects model with inverse-variance weighting using the DerSimonian and Laird method.22 Statistical heterogeneity was quantified using the I2 statistic. An I2 value of 0% represents no heterogeneity, and values of 25%, 50%, and 75% or more represent low, moderate, and high heterogeneity, respectively.23
Results
Literature search
The combined search of Medline, Embase, PubMed, and the Cochrane Library identified 972 abstracts (Figure 1). This included 536 duplicates leaving 436 original abstracts for review. Seventy-four could not be excluded by abstract alone and the full articles were reviewed. A total of 14 articles met the predetermined inclusion criteria. Two articles were subsequently excluded during data analysis as they utilized the same subset of prospectively collected data already included in this review.21,24 The final 12 articles identified for inclusion as outlined above are listed in Table 1.
  | Figure 1 Flow diagram of search strategy to select papers. |
Study and patient characteristics
The level of evidence was unanimously Level IV, consisting of retrospective case series or retrospective cohort studies (Table 1). In the 12 studies, there was a total of 246 patients. Twenty-five patients were lost to follow-up leaving 221 for evaluation. Each study classified the ACJ separation by the Rockwood classification or an equivalent description. The population consisted of 39% type III injuries, 21% type IV injuries, and 40% type V injuries (Table 1). There were no type VI injuries evaluated in any of the included articles. The mean weighted follow-up was 20.4 months (range: 0.5–51 months). The majority of patients in all studies were male (83%–100% of each study) and the mean weighted age was 37.1 years (range: 16–69). Multiple fixation techniques were utilized including synthetic ligament constructs (eg, TightRope, Endobutton), tape (polyester, dacrone, Mersilene), autograft or allograft tendon (GraftRope, gracilis, semitendinosis), Weaver–Dunn reconstructions, and combinations of these techniques. Anatomic and nonanatomic reconstructs were performed.
All patients who underwent fixation using the TightRope technique were treated acutely and accounted for 124 of 221 (56%) of all reconstructions. Less than one-quarter of the patients who underwent allograft/autograft fixation techniques had suffered an acute injury.
Complications
The five most commonly documented complications were infection, shoulder pain, CC calcification, fracture, and loss of reduction (Table 1).
Infection
No deep surgical wounds were observed in any of the study patients. Superficial infections occurred at a pooled rate of 3.8% (95% CI: 0.9%–8.5%; I2=35.4%) in the eight studies describing this complication (Figure 2). Four of the five infections were treated with a short course of oral antibiotics and resolved uneventfully (range: 5 days to 2 weeks). One infection described to be superficial underwent hardware removal with intra-articular washout and debridement.25
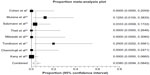  | Figure 2 Pooled rate of infection. |
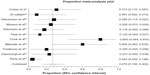
Pain
Eleven articles reported residual shoulder, hardware irritation, or ACJ pain as a postoperative complication with a pooled rate of 26.7% (95% CI: 17.8%–36.6%; I2=57.2%) (Figure 3). Kany et al20 reported six patients who experienced postoperative capsulitis and night pain. Each of these cases ultimately resolved with medical management. Hardware irritation was the most commonly identified source of postoperative pain. Four studies reported hardware irritation rates of 25% or greater.7,25–27 Each of these articles utilized the TightRope fixation technique. Scheibel et al27 reported tenderness over the superior aspect of the implants in eleven patients (39%) with a numeric analogue scale mean of 0.9 points ranging from 0–5.
  | Figure 3 Pooled rate of pain/hardware irritation. |
CC calcification
A total of four studies described CC calcification with a pooled rate of 31.6% (95% CI: 10.1%–58.4%; I2=85.1%) (Figure 4). There was significant variation amongst the different studies ranging from 0% to 85%. Salzmann et al25 identified CC calcification in seven (30.4%) patients. The calcification was present at 6 months and appeared stable with no change at either the 12-month or the 24-month follow-up. Scheibel et al27 reported 19 (67.9%) patients had evidence of calcification in the area of one or both former ligaments. The calcification was graded as mild in five patients, moderate in eleven patients, and severe in three. Patients with severe calcification showed significantly lower CC distance (P<0.05). Patients with mild ossification scored an average of 93% on subjective shoulder value (SSV), 88.4 points in the Constant score (CS), 9.6 points in the Taft score (TF), and 73 points in the acromioclavicular joint instability score (ACJI). Patients with severe ossification scored 96.1% in the SSV, 91.8 points in the CS, 11.3 points in the TF, and 88.9 points in the ACJI. Only ACJI scores were statistically significantly higher (P<0.05).
  | Figure 4 Pooled rate of coracoclavicular calcification. |
Fracture
A total of nine studies reported on coracoid or clavicle fractures. The pooled rate of fracture was 5.3% (95% CI: 2.5%–9.1%; I2=6.2%)(Figure 5). This included seven coracoid fractures and one clavicle fracture. The single clavicle fracture was described by Kany et al20 who attributed this to technical error resulting from multiple passes of the drill through the clavicle during implant positioning. The procedure was converted to an open procedure and the clavicle was plated. A total of seven coracoid fractures were reported (Table 1); the majority (n=6; 87%) of these occurred in patients treated with coracoid tunnel techniques. These occurred in both single and double tunnel techniques. Tomlinson et al17 reported the only coracoid fracture following a coracoid loop fixation technique. This fracture occurred 7-months postoperatively in an active baseball player while pitching.
  | Figure 5 Pooled rate of coracoid or clavicle fracture. |
Loss of reduction
Eleven studies reported loss of reduction with a pooled rate of 26.8% (95% CI: 15.5%–40.0%; I2=73.3%) (Figure 6). This ranged from 6.5% (3/46) by Kany et al20 to 80% (8/10) by Cook et al.10 The rate of dislocation was highest in the studies that had performed graft fixation (the majority of which had chronic ACJ injuries: 26/32; 81.25%).
  | Figure 6 Pooled rate of loss of reduction. |
Cook et al10 reported eight (80%) patients who experienced a significant loss of reduction (three partial; five complete). The average time to loss of reduction was 7 weeks and seven out of eight patients demonstrated intact hardware on the clavicle and coracoid, suggesting a suture breakage/slippage. The remaining patient experienced acute pain at 8 weeks and radiographs demonstrated subsidence of the button through the medial cortex of the coracoid. Four patients underwent revision surgery. The mode of failure confirmed at revision surgery was suture breakage or suture slippage.
Milewski et al28 reported a 60% failure rate using allograft/autograft tendon repairs. Reconstructions were performed using either a coracoid tunnel (n=8; 80%) or coracoid loop (n=2; 20%) autograft techniques. The two patients with a coracoid loop technique did not experience any complications. In the coracoid tunnel group, six of eight patients experienced a loss of reduction, one experienced coracoid fracture requiring revision, and one experienced intraoperative button failure for an overall 100% failure rate in this group.
TightRope fixation techniques were performed in seven studies (Table 1) and comprised 56% of all reconstructions. All cases were performed acutely and a dislocation rate of 8.0% was reported. The rate of hardware migration into the clavicle, the coracoid, or both was as high as 89%.27 However, Scheibel et al reported no correlation between implant migration and CC distance (r=−0.03) or difference (comparison of affected side to normal CC distance) (r=0.08).27 A single study assessed horizontal instability clinically (cross-body test; resisted ACJ compression test) and radiographically (Alexander view: a modified scapular lateral view showing posterior displacement of the clavicle in AC joint injuries).27 An unstable pattern was identified radiographically in 42.9% of cases. These patients had significantly lower taft score (9.2 versus 11.4; P<0.05) and ACJI (63.3 versus 92.3; P<005) scores. The cross-body test and resisted ACJ compression were negative in all patients.
Discussion
The overall rate of serious complications following arthroscopic fixation of the ACJ including infection requiring further surgery or neurovascular compromise were low, while the rate of fracture and loss of reduction remain a concern. Arthroscopic techniques, in general, provide an advantage over open techniques in reducing the rate of surgical-site infection. In the current review, there was a 3.8% superficial infection rate and there were no reported cases of deep infection following arthroscopic ACJ reconstruction. This is consistent with the general arthroscopy literature where the rate of infection has been reported between 0.01% and 0.48%.29 In contrast, open procedures such as hook plate fixation had an overall infection rate of 5% in a recent systematic review.30 This rate increased to over 8% when grafts are used in open reconstructions.31 This considerably higher reported deep infection rate with open ACJ reconstructions should be considered when contemplating ACJ reconstructive surgery. This is particularly relevant when treating controversial grade III ACJ separations where the risk of infection may outweigh the benefits of open ACJ reconstruction and, furthermore, less invasive arthroscopic reconstructions may be advantageous.
The most significant finding of this review was the high rate of failure following arthroscopic allograft or autograft ligament reconstructions (Figure 6). These included reported failure rates of 50% or greater in two independent studies. It should be noted that the majority of these cases were performed in patients suffering from chronic ACJ separations as opposed to acute injuries. Cook et al10 described a complete loss of reduction rate in five of ten patients (50%) with chronic ACJ separations following arthroscopic GraftRope reconstructions. Eighty percent of these failures (four out of five) required surgical revision following this relatively nonanatomic reconstruction. Interestingly, at the time of revision, they observed widening of the clavicle tunnel from 6 mm to an average of 9.6 mm (8.5–12 mm). While the degree of tunnel widening was not correlated with the presence or degree of reduction loss, all four revisions showed tunnel widths greater than 9 mm. The authors suggested that the likely etiology was ongoing motion at the graft–bone interface but that tunnel widening following CC ligament reconstruction required further investigation.
Similarly, Milewski et al28 also reported a high failure rate (60%; six out of ten) following arthroscopic treatment of ten ACJ separations (nine out of ten [90%] chronic) using gracilis or semitendinosis autograft. The majority of patients (seven out of ten; 70%) underwent nonanatomic reconstructions. In this series of patients, the authors correlated their poor results with the use of a coracoid tunnel for distal graft fixation which was performed in 80% (eight out of ten) of the patients. All patients treated by this technique ultimately failed (six loss of reductions, one coracoid fracture, one button failure). In contrast, the two remaining patients who underwent a graft loop technique under the coracoid did not experience a loss of reduction. This is supported by results of Tomlinson et al17 who performed 12 arthroscopic reconstructions in both acute (five out of 12; 42%) and chronic (seven out of 12; 58%) ACJ separations using a graft loop technique under the coracoid. At a mean of 5 months following surgery, two patients had been lost to follow-up. Of the remaining ten patients, 80% had maintained an anatomic reduction. While these results are promising, they may reflect the increased number of acute patients treated in this cohort. Overall, the treatment of chronic ACJ separations remains difficult. Whether using an anatomic or nonanatomic graft, a significant radiographic and clinical failure rate still exists.
The safest and most predictable results for ACJ reconstruction were obtained using TightRope/Endobutton techniques in patients with acute ACJ separation. As stated above, this represented over half of all patients in the current review. While other techniques (eg, Fastak anchors) were used, the TightRope/Endobutton technique was utilized in the majority of acute separations. No chronic ACJ separations were treated with a TightRope/Endobutton technique. The TightRope device evolved using the principles of the Endobutton system.32 Given the similar operative rationale, we grouped these techniques together for assessment in this review. This nonanatomic technique has been recently criticized in biomechanical studies since the vertical placement of the suture fixation device does not replicate the normal direction of the CC ligaments. Therefore, while vertical stability may be restored, horizontal stability (eg, anterior–posterior) may still persist.33 Anatomic reconstruction of both the conoid and trapezoid ligaments using two TightRope devices has led to favorable in vitro results with equal or even higher forces than native ligaments.34
Despite these surgical technique concerns, the TightRope/Endobutton technique had the lowest radiographic failure rate with only 5% of patients demonstrating a recurrent dislocation. It should be reiterated, however, that TightRope/Endobutton procedures were performed exclusively in acute cases and were not used for chronic ACJ reconstructions in this review. Thus, the TightRope/Endobutton technique or similar techniques such as the dog-bone technique35 may prove valuable in treating this particular patient population. Importantly, however, the role of horizontal instability remains unclear. Scheibel et al27 demonstrated that patients with evidence of instability on Alexander views had inferior TF and ACJI scores (P<0.05). However, they reported no difference in SSV or CS and all patients had a negative cross-arm test. Interestingly, these patients were treated with a double TightRope technique shown to be biomechanically stable.34 Furthermore, the effect of more complex suture fixation devices is uncertain (eg, split suture fixation devices).36
When using the TightRope/Endobutton technique, the most commonly reported complication was that of hardware migration into the clavicle, the coracoid, or both. The rate of migration was as high as 89% as reported by Scheibel et al.27 However, these authors found no correlation between implant migration and CC distance (r=−0.03) or difference to the contralateral side (r=0.08). Furthermore, a subsequent publication of the same patient cohort by Venjakob et al21 reported no further migration of the clavicle when final radiographs at 58-months follow-up were compared to the 24-months follow-up radiographs. This suggests that while hardware migration on postoperative radiographs is concerning, it may not indicate eventual clinical or radiographic failure if early ligament healing can be achieved.
When using this technique, however, hardware irritation was a persistent postoperative symptom. In the current review, over one-third of patients treated with TightRope or Endobutton techniques complained of local irritation over the superior clavicle fixation site. Despite the high rate of hardware irritation (~35%), revision surgery for hardware removal was not routinely performed in any study. This is in contrast to open procedures with a hook plate where some degree of pain or discomfort has been reported in all study patients leading to routine second surgeries for hardware removal.37
When performing any ACJ reconstructive procedures, one major concern is that of fracture of the clavicle or coracoid, particularly when bone tunnels are drilled. This complication has been documented in both open and arthroscopic techniques with no obvious increased risk with either approach.28,38 In the current review, seven patients had postoperative coracoid fracture and one patient had a clavicle fracture (pooled rate of fracture: 5.3%). Only a single case of coracoid fracture was reported when the coracoid loop technique17 was utilized. The remainder occurred with bone tunnel drilling techniques.
Some studies have demonstrated a significantly higher perioperative fracture rate.39 In 2013, Martetschlager et al39 reviewed the complications following anatomic ACJ reconstruction (using both open and arthroscopic techniques). These authors demonstrated a 20% combined fracture rate (ie, of the clavicle and coracoid) and related the complication to the technical errors in drilling technique. Of particular importance was that good to excellent outcomes were only reported in those patients who did not experience such a complication and, therefore, avoidance of this complication either by careful placement of bone tunnels or utilizing a loop technique should be strongly considered. This study was not included in the current review as it utilized a mix of open and arthroscopic techniques and the arthroscopic data could not be extracted from the open data, resulting in exclusion.
In the study by Milewski et al,28 perioperative fractures occurred during both arthroscopic and open repairs. Overall, they demonstrated an 18.5% fracture rate (five of 27 patients), although only a 10% fracture rate (one of ten arthroscopic patients) when an arthroscopic technique was utilized. While the difference may be related to open versus arthroscopic techniques, these authors related these fractures (particularly clavicle fractures) to technical errors. They suggested that both a wider distance between tunnels and from the tunnel to the lateral edge of the clavicle may help decrease the risk of clavicle fracture.28
Clearly, clavicle and coracoid fractures are significant, should be avoided, and are likely related to bone tunnel location, size, and proximity to the distal clavicle or other bone tunnels. While there is no evidence to support specific parameters that eliminate coracoid or clavicle fractures, care should be taken intraoperatively to ensure accurate placement of bony tunnels through the center of the bone on a single pass and to maximize the distance between other bony tunnels and the terminal bone end. In the current review, the overall fracture rate was significant at 5.3%.
While overall the results of the current review suggest that arthroscopic ACJ reconstruction have a distinct complication profile, a number of significant limitations exist. First, the results of this review are based on Level IV evidence and no randomized controlled trials or comparative series were included. Furthermore, comparison between anatomic versus nonanatomic techniques remains sparse. Similarly, we were unable to divide acute and chronic reconstructions for statistical analysis as only a single study performed exclusively chronic reconstructions. However, the purpose of this study was to determine the overall complication rate of arthroscopic ACJ reconstructions only. Second, the mean follow-up of the included studies was only 20.4 months, and, therefore, the overall long-term complication rate in particular related to loss of reduction is unclear. However, some studies have demonstrated minimal radiographic changes between short- and long-term follow-up.21 Finally, complications in multiple previous studies of surgical procedures have been associated with surgeon experience.40,41 We attempted to minimize this effect by including only studies with greater than ten patients. However, when performing a new and relatively technically demanding procedure, it is unclear what the overall learning curve may be.
Conclusion
In conclusion, arthroscopic ACJ reconstruction techniques are relatively safe procedures but demonstrate a distinct complication profile. The TightRope/Endobutton technique, when performed in patients with acute ACJ separations, demonstrated good radiographic outcomes with a high rate of hardware irritation. In contrast, graft reconstructions in patients with chronic ACJ dislocations demonstrated variable results with a high risk for loss of reduction. Coracoid/clavicle fractures remain a significant complication that occur predominately in techniques utilizing bone tunnels. Further research is required to determine long-term outcomes and if modifications of technique may be helpful in improving outcomes or minimizing complications.
Disclosure
The authors report no conflicts of interest in this work.
References
Bradley JP, Elkousy H. Decision making: operative versus nonoperative treatment of acromioclavicular joint injuries. Clin Sports Med. 2003;22(2):277–290. | |
Tossy JD, Mead NC, Sigmond HM. Acromioclavicular separations: useful and practical classification for treatment. Clin Orthop Relat Res. 1963;28:111–119. | |
Williams GR, Nguyen VD, Rockwood CR. Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol. 1989;18:29–34. | |
Cox JS. The fate of the acromioclavicular joint in athletic injuries. Am J Sports Med. 1981;9(1):50–53. | |
Simovitch R, Sanders B, Ozbaydar M, Lavery K, Warner JJ. Acromioclavicular joint injuries: diagnosis and management. J Am Acad Orthop Surg. 2009;17(4):207–219. | |
Rios CG, Mazzocca AD. Acromioclavicular joint problems in athletes and new methods of management. Clin Sports Med. 2008;27(4):763–788. | |
Cohen G, Boyer P, Pujol N, Hamida Ferjani B, Massin P, Hardy P. Endoscopically assisted reconstruction of acute acromioclavicular joint dislocation using a synthetic ligament. Outcomes at 12 months. Orthop Traumatol Surg Res. 2011;97(2):145–151. | |
Bishop JY, Kaeding C. Treatment of the acute traumatic acromioclavicular separation. Sports Med Arthrosc. 2006;14(4):237–245. | |
Rolla PR, Surace MF, Murena L. Arthroscopic treatment of acute acromioclavicular joint dislocation. Arthroscopy. 2004;20(6):662–668. | |
Cook JB, Shaha JS, Rowles DJ, Bottoni CR, Shaha SH, Tokish JM. Early failures with single clavicular transosseous coracoclavicular ligament reconstruction. J Shoulder Elbow Surg. 2012;21(12):1746–1752. | |
Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007;35(2):316–329. | |
Geaney LE, Miller MD, Ticker JB, et al. Management of the failed AC joint reconstruction: causation and treatment. Sports Med Arthrosc. 2010;18(3):167–172. | |
Salzmann GM, Walz L, Schoettle PB, Imhoff AB. Arthroscopic anatomical reconstruction of the acromioclavicular joint. Acta Orthop Belg. 2008;74(3):397–400. | |
Wolf EM, Pennington WT. Arthroscopic reconstruction for acromioclavicular joint dislocation. Arthroscopy. 2001;17(5):558–563. | |
Struhl S. Double Endobutton technique for repair of complete acromioclavicular joint dislocations. Techniques in Shoulder and Elbow Surgery. 2007;8 (4):175–179. | |
Lafosse L, Baier GP, Leuzinger J. Arthroscopic treatment of acute and chronic acromioclavicular joint dislocation. Arthroscopy. 2005; 21(8):1017. | |
Tomlinson DP, Altchek DW, Davila J, Cordasco FA. A modified technique of arthroscopically assisted AC joint reconstruction and preliminary results. Clin Orthop Relat Res. 2008;466(3):639–645. | |
DeBerardino TM, Pensak MJ, Ferreira J, Mazzocca AD. Arthroscopic stabilization of acromioclavicular joint dislocation using the AC graftrope system. J Shoulder Elbow Surg. 2010;19(Suppl 2):47–52. | |
Defoort S, Verborgt O. Functional and radiological outcome after arthroscopic and open acromioclavicular stabilization using a double-button fixation system. Acta Orthop Belg. 2010;76(5):585–591. | |
Kany J, Amaravathi RS, Guinand R, Valenti P. Arthroscopic acromioclavicular joint reconstruction using a synthetic ligament device. Eur J Orthop Surg Traumatol. 2012;22(5):357–364. | |
Venjakob AJ, Salzmann GM, Gabel F, et al. Arthroscopically assisted 2-bundle anatomic reduction of acute acromioclavicular joint separations: 58-month findings. Am J Sports Med. 2013;41(3):615–621. | |
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. | |
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. | |
Kraus N, Haas NP, Scheibel M, Gerhardt C. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations in a coracoclavicular Double-TightRope technique: V-shaped versus parallel drill hole orientation. Arch Orthop Trauma Surg. 2013;133(10):1431–1440. | |
Salzmann GM, Walz L, Buchmann S, Glabgly P, Venjakob A, Imhoff AB. Arthroscopically assisted 2-bundle anatomical reduction of acute acromioclavicular joint separations. Am J Sports Med. 2010;38(6):1179–1187. | |
Glanzmann MC, Buchmann S, Audigé L, Kolling C, Flury M. Clinical and radiographical results after double flip button stabilization of acute grade III and IV acromioclavicular joint separations. Arch Orthop Trauma Surg. 2013;133(12):1699–1707. | |
Scheibel M, Dröschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39(7):1507–1516. | |
Milewski MD, Tompkins M, Giugale JM, Carson EW, Miller MD, Diduch DR. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40(7):1628–1634. | |
Babcock HM, Matava MJ, Fraser V. Postarthroscopy surgical site infections: review of the literature. Clin Infect Dis. 2002;34(1):65–71. | |
Modi CS, Beazley J, Zywiel MG, Lawrence TM, Veillette CJ. Controversies relating to the management of acromioclavicular joint dislocations. Bone Joint J. 2013;95-B(12):1595–1602. | |
Tauber M, Gordon K, Koller H, Fox M, Resch H. Semitendinosus tendon graft versus a modified Weaver-Dunn procedure for acromioclavicular joint reconstruction in chronic cases: a prospective comparative study. Am J Sports Med. 2009;37(1):181–190. | |
Lim YW, Sood A, van Riet RP, Bain GI. Acromioclavicular joint reduction, repair and reconstruction using metallic buttons – early results and complications. Techniques in Shoulder and Elbow Surgery. 2007;8(4):213–221. | |
Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2):236–246. | |
Walz L, Salzmann GM, Fabbro T, Eichhorn S, Imhoff AB. The anatomic reconstruction of acromioclavicular joint dislocations using 2 TightRope devices: a biomechanical study. Am J Sports Med. 2008;36(12):2398–2406. | |
Braun S, Imhoff AB, Martetschlaeger F. Primary fixation of acromioclavicular joint disruption. Oper Tech Sports Med. 2014;22(3):221–226. | |
Lädermann A, Gueorguiev B, Stimec B, Fasel J, Rothstock S, Hoffmeyer P. Acromioclavicular joint reconstruction: a comparative biomechanical study of three techniques. J Shoulder Elbow Surg. 2013;22(2):171–178. | |
Ejam S, Lind T, Falkenberg B. Surgical treatment of acute and chronic acromioclavicular dislocation Tossy type III and V using the Hook plate. Acta Orthop Belg. 2008;74(4):441–445. | |
Turman KA, Miller CD, Miller MD. Clavicular fractures following coracoclavicular ligament reconstruction with tendon graft: a report of three cases. J Bone Joint Surg Am. 2010;92(6):1526–1532. | |
Martetschlager F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41(12):2896–2903. | |
Hammond JW, Queale WS, Kim TK, McFarland EG. Surgeon experience and clinical and economic outcomes for shoulder arthroplasty. J Bone Joint Surg Am. 2003;85-A(12):2318–2324. | |
Jain NB, Kuye I, Higgins LD, Warner JJ. Surgeon volume is associated with cost and variation in surgical treatment of proximal humeral fractures. Clin Orthop Relat Res. 2013;471(2):655–664. | |
El Sallakh SA. Evaluation of arthroscopic stabilization of acute acromioclavicular joint dislocation using the TightRope system. Orthopedics. 2012;35(1):e18–e22. | |
Murena L, Vulcano E, Ratti C, Cecconello L, Rolla PR, Surace MF. Arthroscopic treatment of acute acromioclavicular joint dislocation with double flip button. Knee Surg Sports Traumatol Arthrosc. 2009; 17(12):1511–1515. | |
Thiel E, Mutnal A, Gilot GJ. Surgical outcome following arthroscopic fixation of acromioclavicular joint disruption with the tightrope device. Orthopedics. 2011;34(7)e267–e274. | |
Chernchujit B, Tischer T, Imhoff AB. Arthroscopic reconstruction of the acromioclavicular joint disruption: surgical technique and preliminary results. Arch Orthop Trauma Surg. 2006;126(9):575–581. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

