Back to Journals » Clinical Ophthalmology » Volume 8
Comparison of the effect of W-shaped and linear skin incisions on scar visibility in bilateral external dacryocystorhinostomy
Authors Ekinci M, Çağatay HH, Gokce G, Ceylan E, Keleş S, Çakici O, Oba ME, Yazar Z
Received 11 November 2013
Accepted for publication 12 December 2013
Published 20 February 2014 Volume 2014:8 Pages 415—419
DOI https://doi.org/10.2147/OPTH.S57382
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Metin Ekinci,1 Halil Hüseyin Çağatay,1 Gokcen Gokce,2 Erdinç Ceylan,3 Sadullah Keleş,4 Özgür Çakici,5 Mehmet Ersin Oba,1 Zeliha Yazar1
1Department of Ophthalmology, University of Kafkas, 2Department of Ophthalmology, Sarikamis Military Hospital, Sarikamis, Kars, 3Ophthalmology Clinic, Erzurum Training and Research Hospital, 4Department of Ophthalmology, University of Atatürk, Erzurum, 5Department of Ophthalmology, University of Mugla Sitki Kocman, Muğla, Turkey
Background: The aim of this study was to compare the effect of W-shaped skin (WS) and linear skin (LS) incisions on cutaneous scar tissue formation in patients who have undergone bilateral external dacryocystorhinostomy.
Methods: Sixteen patients (14 females and two males) with acquired bilateral nasolacrimal duct obstruction were included in this prospective, interventional comparative study. LS incision was applied to one side and WS skin incision to the other side. The skin incisions were assessed 6 months after each procedure by the patients themselves and by two ophthalmologists who were unaware of the skin incision shape and side. Scar tissue that was not recognized under the same light conditions and in the same room from a 100 cm distance was recorded as grade 1. Minimally visible scar tissue was assessed as grade 2, moderately visible scar tissue as grade 3, and easily visible scar tissue as grade 4.
Results: The mean scar assessment scores recorded by the first ophthalmologist were 2.50±0.82 for the LS group and 1.25±0.45 for the WS group (P<0.001). The second ophthalmologist’s assessment scores were 2.25±0.86 for the LS group and 1.25±0.45 for the WS group (P<0.001). The mean patient self-assessment score for the incision scars was 2.44±1.03 for the LS group and 1.56±0.73 for the WS group (P<0.001).
Conclusion: Compared with LS incision, WS incision resulted in less cutaneous scar tissue formation in patients who have undergone bilateral external dacryocystorhinostomy.
Keywords: external dacryocystorhinostomy, skin, W-shaped incision, linear incision
A Letter to the Editor has been received and published for this article
Introduction
Since its introduction in 1904 by Toti, external dacryocystorhinostomy (E-DCR) has been the gold standard in the management of acquired nasalacrimal duct obstruction.1 E-DCR is a cost-effective surgical technique that may be performed under local anesthesia with minimal blood loss.2–8 As an alternative to E-DCR, other surgical techniques involving no skin incision but with increased cost, such as endoscopic endonasal laser-assisted dacryocystorhinostomy, mechanical endoscopic endonasal dacryocystorhinostomy, and laser endocanalicular dacryocystorhinostomy have been performed, with variable success rates in modern nasolacrimal duct obstruction surgery. These techniques have the potential to enable simultaneous surgery for associated nasal pathology and to decrease the postoperative recovery time.9–11
E-DCR has a high surgical success rate but scar tissue formation at the incision site may be a major drawback for patients.9–14 A linear skin (LS) incision medial to the angular vessels or a curvilinear incision are techniques used in E-DCR. There have been few studies comparing the visibility of E-DCR scars. Devoto et al reported that 9% of their patients who had undergone E-DCR graded the incision scar as very visible and 26% graded it as moderately visible.13 We believe that an incision shape that takes into account cutaneous stress lines may be effective in reducing formation of scar tissue. Therefore, in this study, we aimed to compare the effect of W-shaped (WS) and LS incisions on cutaneous scar tissue formation in patients who have undergone bilateral E-DCR.
Materials and methods
Sixteen Caucasian patients (14 female and two male) of mean age 40.8±14.3 (range 21–65) years who underwent bilateral E-DCR between June 2011 and June 2012 were included in this prospective, interventional, comparative study. Approval was obtained from the Kafkas University ethics committee (approval number 12/2011). The diagnosis of acquired nasalacrimal duct obstruction was clinically confirmed by preoperative lacrimal probing and lavage. All patients were aware of the endonasal approach and informed consent for E-DCR was obtained from each patient. All patients were assessed preoperatively by an otorhinolaryngologist for any intranasal pathology. If there was concomitant intranasal pathology (eg, synechiae, deviated septum), an intranasal, endoscopic approach was suggested and the patient was excluded from the study. Patients with canalicular/common canalicular obstruction, a history of trauma, acute dacryocystitis with a history of fistulization, or a skin disorder that might affect the process of wound healing were also excluded. All surgeries were performed under local anesthesia with sedation by the same experienced surgeon (ME). An LS incision was applied to one side and a WS incision to the other side. The skin incisions were assessed 6 months after each procedure by the patients themselves and by two ophthalmologists who were unaware of the skin incision shape and side.
Surgical procedure
All patients were operated on using the same surgical protocol. The LS incision was 12 mm in length and 8 mm medial to the medial canthus, with one third of the incision (4 mm) lying above the medial canthal angle15 (Figure 1A). The WS skin incision was 12 mm in linear length. The W shape was formed by three consecutive equilateral triangles having sides 4 mm in length with two tips and one base that showed the medial canthus (Figure 1B). Except for the difference in shape of the skin incision, the surgical dissection technique was the same in all patients. The orbicularis muscle was dissected. After reaching the periosteum, the anterior lacrimal crest was exposed, with elevation of the periosteum. The lacrimal sac was inflated with irrigation and its borders were defined. It was pushed laterally with a periosteal elevator, and the osteotomy was performed and expanded with rongeur. H-shaped flaps were prepared on the lacrimal sac and nasal mucosa. The anterior and posterior flaps were sutured with two separate 6/0 Vicryl sutures, creating an anastomosis between the lacrimal sac and the nasal cavity. The subcutaneous tissues were sutured with three 6/0 Vicryl sutures, and the skin incisions were sutured with 6/0 Prolene. The LS incisions were closed using four separate sutures and the WS incisions with five separate sutures placed at the tips and gaps of the triangles that had been formed by the incisions. There were no perioperative problems (such as excessive bleeding as a result of angular vessel damage, injury of the posterior part of the medial canthal tendon, or injury of the lateral nasal wall) or postoperative complications in either group.
  | Figure 1 Shape of incisions. (A) Linear skin incision and (B) W-shaped incision. |
Postoperative evaluation and scar assessment
Postoperatively, all patients received the same topical antibiotic drops and ointment for 2 weeks and the same vasoconstrictor nasal spray for 5 days. The sutures were removed on postoperative day 10 in both groups. The patients were examined on postoperative day 1, and then at day 10 and one and 6 months postoperatively. Lacrimal function was evaluated at each examination. The surgeries were not simultaneous, so assessment of scar visibility on each side was done at the 6-month postoperative visit to prevent one side being more healed than the other at evaluation. The skin incision scar was photographed for archiving purposes only. The scar was assessed and scored by direct visualization of the tissue under the same light conditions and in the same room from a 100 cm distance using the modified scoring system described by Devoto et al.13 Using this assessment method, scar tissue that was not recognized under the same light conditions in the same room from a 100 cm distance was recorded as grade 1, even if it was noticeable by both the patient and surgeon on close examination. Minimally visible scar tissue was assessed as grade 2, moderately visible scar tissue as grade 3, and easily visible scar tissue as grade 4.
Statistical analysis
Statistical Package for the Social Sciences version 16.0 software (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis, specifically the nonparametric Wilcoxon signed rank and chi-squared tests. A P-value <0.05 was accepted as being statistically significant.
Results
The study population comprised 14 female (87.5%) and two male (12.5%) patients of mean age 40.8±14.3 (21–65) years. The mean scar assessment scores recorded by the first ophthalmologist were 2.50±0.82 for the LS group and 1.25±0.45 for the WS group (P<0.001). The mean scar assessment scores given by the second ophthalmologist were 2.25±0.86 for the LS group and 1.25±0.45 for the WS group (P<0.001). Patient self-assessment scores for the incision scars were 2.44±1.03 for the LS group and 1.56±0.73 for the WS group (P<0.001, Table 1 and Figure 2).
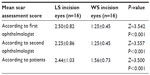  | Table 1 Mean scar incision assessment scoring by ophthalmologists and patients |
Discussion
Incisional scar tissue after E-DCR may represent a cosmetic problem for patients. In this study, we investigated the effect of skin incision shape on the degree of scar visibility. To the best of our knowledge, this is the first study investigating scar visibility in patients who have undergone bilateral E-DCR.
Langer et al described the normal tensile strength lines of the skin and reported that the direction of the incision line was one of the most important factors determining final scar formation.16 Borges emphasizes the importance of obtaining relaxed tensile strength lines at the skin incision17 and recommends that the incision should be performed parallel to the tensile strength lines. When the final tensile strength of the long line of the incision (relaxed skin tension line) is minimized, scar formation is optimized. The wrinkle lines are placed perpendicular to the underlying muscles and are on the same plane as the relaxed tensile lines.16–18 In the present study, we performed all of our skin incisions perpendicular to the underlying orbicularis muscle on the relaxed skin tension line and obtained minimal tensile strength at the wound lips. Minimal tensile strength would imply minimal scar formation.
During cosmetic surgical interventions in the periorbital, perioral and nasolabial areas, the same basic principles are applied using the well known Z-plasty and S-plasty reparative techniques in order to relax the tensile forces at the wound edges where the skin is resistant.19 The WS incision may be considered as a modified form of Z-plasty, and our study shows that it is effective in reducing incisional scarring by relaxing skin tension in patients undergoing E-DCR. The precautions reported in the literature20–24 should be followed in order to reduce incision scar formation in E-DCR.
In the literature, skin incisions other than WS and LS have been described for E-DCR.25–29 Satisfactory results have been reported with the LS incision. Devoto et al used the LS incision in their patients, which was evaluated by the patients themselves and by an ophthalmologist; they reported that the scar was unremarkable or minimally visible in 91% of their patients.13 Sharma et al30 scored LS incision scars in their patients from 1 to 5, and reported a score of ≥1 in 10.5% of cases and a score ≥2 in only 4%. Caesar et al31 reported a study in which 67% of their patients described the incision scar as “invisible” and 97% were happy with their scar. In our study, the mean LS incision scores given by the patients and two ophthalmologists were 2.44±1.03, 2.50±0.82, and 2.25±0.86, respectively. When compared with the literature, these values seem to be high, and may reflect the younger age of our patients. The mean age in our study was 40.8±14.3 years versus 67 years in the study reported by Sharma et al, 61 in that reported by Devoto et al, and 62 in that reported by Caesar et al.13,30,31 Further, Kearney et al detected more pronounced scarring in young patients.32 Caesar et al suggested that the high scores in younger patients may come from their otherwise smoother and less flawed skin and good visual acuity, which allows them to observe scar formation more easily.31
The WS incision may have some limitations and disadvantages, in particular the length of incision, in that the classical LS incision is 12 mm while the WS incision is 24 mm. The edge redundancy in WS incisions may make subcutaneous dissection more difficult in comparison with LS incisions. The edges of the WS incision can be easily damaged during surgery. Suturing time during WS incision wound closure results in a longer operation time. Additionally, the WS incision carries a risk of vascular compromise to the tips of the very small flaps, especially in the limited space of the medial canthus and lateral nasal wall. Further, there might be a limitation of WS incisions related to the nasal anatomy of the patient. Depending on the nasal projection and broadness of the nasal bridge, the medial limb of the WS incision may extend too far anteriorly, causing more visible and disfiguring scar formation. In our study, WS incisions were performed in patients of Caucasian origin with a relatively high nasal bridge.
An ideal E-DCR is one where there is a large bony ostium and good mucosal anastomosis without an external scar.25 The curvilinear incision avoids scar formation as far as possible, and follows the relaxed skin tension lines better and with less webbing in E-DCR. However, unlike the linear incision, the curvilinear incision cannot be easily extended superiorly to allow more superior bone removal (without damaging the cribriform plate), maintain an adequate anastomosis, or increase surgical success. In our experience, this limitation may be a problem and is why the classic curvilinear incision was not used instead of LS incision in our study. On the other hand, using a lazy S or curvilinear incision, rather than a linear incision, may have been more clinically meaningful in terms of scar visibility and this is the major limitation of our study. Additionally, scar assessment at 6 months may be inadequate because scars need at least a year to mature and reach their best appearance. Our results need to be confirmed by further long-term studies comparing the WS incision with lazy S or curvilinear incisions.
In conclusion, as in our previous study,33 which included two separate patient groups, this study minimized patient-related factors by performing LS and WS incisions in the same patient group, and shows that WS incision is a good alternative to LS incision for reducing scar formation after E-DCR. Further studies are needed to confirm our findings.
Disclosure
The authors report no conflicts of interest in this work.
References
Watkins LM, Janfaza P, Rubin PAD. Evolution of endonasal dacryocystorhinostomy. Surv Ophthalmol. 2003;48:73–84. | |
Bartley GB. The pros and cons of laserdacryocystorhinostomy. Am J Ophthalmol. 1994;117:103–106. | |
Warren JF, Seiff SR, Kavanagh MC. Long-term results of external dacryocystorhinostomy. Ophthalmic Surg Lasers Imaging. 2005;36:446–450. | |
Erdol H, Akyol N, Imamoglu HI, Sozen E. Long-term follow-up of external dacryocystorhinostomy and the factors affecting its success. Orbit. 2005;24:99–102. | |
Yazici B, Yazici Z. Final nasolacrimal ostium after external dacryocystorhinostomy. Arch Ophthalmol. 2003;121:76–80. | |
Benger R. Day-surgery external dacryocystorhinostomy. Aust N Z J Ophthalmol. 1992;20:243–245. | |
Jordan DR. Avoiding blood loss in outpatient dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 1991;7:261–266. | |
Ciftci F, Pocan S, Karadayi K, Gulecek O. Local versus general anesthesia for external dacryocystorhinostomy in young patients. Ophthal Plast Reconstr Surg. 2005;21:201–206. | |
Woog JJ, Kennedy RH, Custer PL, et al. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2001;108:2369–2377. | |
Tarbet KJ, Custer PL. External dacryocystorhinostomy. Surgical success, patient satisfaction, and economic cost. Ophthalmology. 1995;102:1065–1070. | |
Walker RA, Al-Ghoul A, Conlon MR. Comparison of nonlaser nonendoscopic endonasal dacryocystorhinostomy with external dacryocystorhinostomy. Can J Ophthalmol. 2011;46:191–195. | |
Sharma B. Non endoscopic endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Kathmandu Univ Med J (KUMJ). 2008;6:437–442. | |
Devoto MH, Zaffaroni MC, Bernardini FP, de Conciliis C. Postoperative evaluation of skin incision in external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2004;20:358–361. | |
Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology. 2003;110:78–84. | |
Olver JM. Tips on how to avoid the DCR scar. Orbit. 2005;24:63–66. | |
Langer K. On the anatomy and physiology of the skin. The cleavability of the cutis. Br J Plast Surg. 1978;31:3–8. | |
Borges AF. Relaxed skin tension lines. Dermatol Clin. 1989;7:169–177. | |
CH Thorne. Techniques and principles in plastic surgery. In: Charles H Thorne, editor. Grabb and Smith’s Plastic Surgery. 7th ed. Philadelphia, PA, USA: Lippincott Williams & Wilkins; 2007. | |
Reish RG, Eriksson E. Scar treatments: preclinical and clinical studies. J Am Coll Surg. 2008;206:719–730. | |
Dortzbach R, Woog JJ. Small-incision techniques in ophthalmic plastic surgery. Ophthalmic Surg. 1990;21:615–622. | |
Caesar RH, McNab AA. External dacryocystorhinostomy and local anaesthesia: techniques to measure minimised blood loss. Ophthal Plast Reconstr Surg. 2004;20:57–59. | |
Niessen FB, Spauwen PH, Kon M. The role of suture material in hypertrophic scar formation: Monocryl vs Vicryl-rapide. Ann Plast Surg. 1997;39:254–260. | |
Yazici B, Meyer DR. Selective antibiotic use to prevent postoperative wound infection after external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2002;18:331–334. | |
Ciftci F, Dinc UA, Ozturk V. The importance of lacrimal diaphragm and periosteum suturation in externaldacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2010;26:254–258. | |
Dave TV, Javed Ali M, Sravani P, Naik MN. Subciliary incision for external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2012;28:341–345. | |
Adenis J-P, Robert P-Y. Retrocanalicular approach to the medial orbit for dacryocystorhinostomy. Graefes Arch Clin Exp Ophthalmol. 2003;241:725–729. | |
Gutman J, Shinder R. Re: “Transconjunctival dacryocystorhinostomy: scarless surgery without endoscope and laser assistance”. Ophthal Plast Reconstr Surg. 2011;27:465–466. | |
Mjarkesh MM, Morel X, Renard G. [Study of the cutaneous scar after external dacryocystorhinostomy]. J Fr Ophtalmol. 2012;35:88–93. French. | |
Kaynak-Hekimhan P, Yilmaz OF. Transconjunctival dacryocystorhinostomy: scarless surgery without endoscope and laser assistance. Ophthal Plast Reconstr Surg. 2011;27:206–210. | |
Sharma V, Martin PA, Benger R, et al. Evaluation of the cosmetic significance of external dacryocystorhinostomy scars. Am J Ophthalmol. 2005;140:359–362. | |
Caesar RH, Fernando G, Scott K, McNab AA. Scarring in external dacryocystorhinostomy: fact or fiction? Orbit. 2005;24:83–86. | |
Kearney CR, Holme SA, Burden AD, McHenry P. Longterm patient satisfaction with cosmetic outcome of minor cutaneous surgery. Australas J Dermatol. 2001;42:102–105. | |
Ekinci M, Caǧatay HH, Oba ME, et al. The long-term follow-up results of external dacryocystorhinostomy skin incision scar with “w incision”. Orbit. 2013;32(6):349–355. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

