Back to Journals » OncoTargets and Therapy » Volume 8
Associations between deepness of response and clinical outcomes among Japanese patients with metastatic colorectal cancer treated with second-line FOLFIRI plus cetuximab
Authors Osumi H , Matsusaka S, Suenaga M , Shinozaki E, Mizunuma N
Received 22 April 2015
Accepted for publication 9 June 2015
Published 6 August 2015 Volume 2015:8 Pages 2005—2013
DOI https://doi.org/10.2147/OTT.S87101
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Daniele Santini
Hiroki Osumi, Satoshi Matsusaka, Mitsukuni Suenaga, Eiji Shinozaki, Nobuyuki Mizunuma
Department of Gastroenterology, Cancer Institute Hospital, Japanese Foundation for Cancer Research, Tokyo, Japan
Background: In the FIRE-3 trial, overall survival (OS) was significantly longer in patients treated with FOLFIRI plus cetuximab (C-mab) than in those treated with FOLFIRI plus bevacizumab (Bev), but progression-free survival (PFS) was not significantly different. This may be associated with the deepness of response (DpR) in patients treated with FOLFIRI plus C-mab. We aimed to evaluate the relationship between clinical outcome and DpR in metastatic colorectal cancer (mCRC) patients treated with second-line FOLFIRI plus C-mab.
Methods: A total of 112 patients with histopathologically confirmed mCRC treated with second-line FOLFIRI in combination with C-mab (N=42) or Bev (N=70) were retrospectively enrolled between October 2008 and June 2013. The relationship between DpR and clinical outcome in patients treated with FOLFIRI plus C-mab or Bev was determined.
Results: Forty-two patients treated with FOLFIRI plus C-mab had a mean DpR of 6.1% (interquartile range: -13.7%, 20.8%) and a minimum DpR of -62.7%. On the other hand, 70 patients treated with FOLFIRI plus Bev had a mean DpR of 0% (interquartile range: -16%, 10%) and a minimum DpR of -111%. DpR ≥30% was associated with significantly longer OS and PFS when compared with DpR ≤30% in patients given FOLFIRI plus C-mab. DpR (≥30%) was independently associated with prolongation of OS and PFS. In patients treated with FOLFIRI plus C-mab, there was a moderate positive correlation between DpR and clinical outcomes (OS: r=0.51, P<0.001; PFS: r=0.54, P<0.001).
Conclusion: FOLFIRI plus C-mab yielded a stronger correlation between DpR and clinical outcomes. These results indicate the potential of DpR as a new measure of efficacy in mCRC patients treated with second-line chemotherapy plus C-mab.
Keywords: deepness of response, second-line chemotherapy, cetuximab, metastatic colorectal cancer
Introduction
In metastatic colorectal cancer (mCRC) patients, it is assumed that patients receiving first-line chemotherapy will get second-line chemotherapy. The E3200 study showed the addition of bevacizumab (Bev) to oxaliplatin, fluorouracil, and leucovorin improves survival duration for patients with previously treated mCRC.1 Furthermore, the BRiTE2 and ML181473 studies also showed that continuous use of Bev throughout second-line chemotherapy prolonged overall survival (OS) and progression-free survival (PFS). On the other hand, the EPIC4 study and a trial of FOLFIRI plus panitumumab (P-mab) compared with FOLFIRI alone after the failure of initial treatment in mCRC patients with KRAS wild-type tumors5 showed that second-line cetuximab (C-mab) or P-mab only prolonged PFS. However in the SPIRITT (study 20060141) trial,6 a randomized Phase II study of FOLFIRI with either P-mab or Bev as second-line treatment in patients with KRAS wild-type mCRC, efficacy was not significantly different between the P-mab plus FOLFOX or FOLFIRI regimens and Bev plus FOLFOX or FOLFIRI. As mentioned above, because several Phase III trials showed that standard chemotherapy plus Bev contributed to prolongation of both OS and PFS, the first choice of second-line treatment was standard chemotherapy plus Bev, but standard chemotherapy plus anti-EGFR inhibitor can be the alternative treatment choice.
A randomized AIO study in Germany, KRK-0306 (FIRE-3), of FOLFIRI plus C-mab versus FOLFIRI plus Bev in first-line treatment of KRAS wild-type mCRC found no significant difference in overall response rate or PFS. OS, however, was significantly longer in patients treated with FOLFIRI plus C-mab than in those with FOLFIRI plus Bev.7 One of the main reasons that OS was prolonged in the C-mab group may have been the deepness of response (DpR) elicited by first-line treatment with C-mab. DpR is the percentage of tumor shrinkage observed at the nadir compared with baseline. The concept of DpR concerns the relationship between tumor shrinkage and post-progression survival.8 It has been suggested that DpR can act as a surrogate marker of OS in patients treated with first-line chemotherapy plus C-mab.
It is unclear whether DpR can also be applied in mCRC patients treated with second-line C-mab-based chemotherapy and whether second-line chemotherapy plus C-mab or Bev yields a better correlation between DpR and clinical outcome. The purpose of this retrospective analysis was to determine whether there was a relationship between clinical outcome and DpR in patients treated with second-line FOLFIRI plus C-mab.
Methods
A total of 112 patients with histopathologically confirmed mCRC treated with first-line FOLFOX/XELOX in combination with Bev and second-line FOLFIRI with C-mab (N=42) or Bev (N=70) were enrolled between October 2008 and June 2013. This study has been performed in accordance with the Declaration of Helsinki. Our Institutional Review Board approved this study (Registry number: 1544). We obtained comprehensive written informed consent about the research before chemotherapy was started.
Treatment evaluation
OS was defined as the time from the 1st day of treatment to death from any cause. PFS was defined as the time from the 1st day of treatment to either the first objective evidence of disease progression or to death from any cause. Tumor response was assessed by the investigator using computed tomography every 8 weeks (±2 weeks) until disease progression. Disease progression was defined as an increase in the sum of the longest tumor diameters by 20% or more, as compared with before treatment. This definition of disease progression makes use of the SOFT trial. DpR was defined as the maximum reduction ratio compared with baseline tumor regardless of the period.
Data collection
All dates were identified by review of medical records and/or imaging. Prognostic factors included age (<65 or ≥65 years old), sex (male or female), performance status (PS; 0 or 1), site of metastasis (liver, lung, lymph node, peritoneum), multiple metastases (yes or no), number of metastasis (one or other), tumor location (left or right), DpR (≥ mean%, ≥20%, ≥30%). KRAS status was evaluated by Luminex assays. The sensitivity of KRAS testing by Luminex has been reported to be 10%.9
Statistical analysis
OS and PFS were estimated using the Kaplan–Meier method and compared using the log-rank test. All reported P-values were the result of two-sided tests, with P<0.05 considered statistically significant. Prognostic factors showing P<0.2 in the univariate analysis were included in the multivariate analysis. Correlations between DpR and clinical outcome were estimated using Pearson’s correlation coefficient. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing).
Results
Patient characteristics
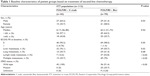
A total of 112 patients were enrolled between October 2008 and June 2013 (Table 1). All patients were treated with FOLFIRI as second-line chemotherapy. Seventy patients (62.5%) received Bev. Forty-two patients (37.5%) received C-mab with FOLFIRI. There were significant differences in sex, liver metastasis, lymph node metastasis, multiple metastasis, and KRAS status observed in the baseline clinical characteristics between the two groups. The median duration of follow-up at the time of this analysis was 13.6 months (1.6–39.7 months).
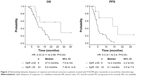
Correlations between DpR and clinical outcome
In patients treated with FOLFIRI plus C-mab as second-line chemotherapy, there was moderate positive correlation between DpR and clinical outcomes (OS: r=0.51, P<0.001; PFS: r=0.54, P<0.001). Meanwhile, in patients treated with FOLFIRI plus Bev as second-line chemotherapy, there was minor negative correlation between DpR and OS, and minor positive correlation between DpR and PFS (OS: r=-0.35, P=0.002; PFS: r=0.39, P<0.001) (Figure 1).
Forty-two patients treated with FOLFIRI plus C-mab had a mean DpR of 6.1% (interquartile range: −13.7%, 20.8%) and a minimum DpR of −62.7%. The median period until maximum shrinkage was 14 weeks (±11.3). On the other hand, 70 patients treated with FOLFIRI plus Bev had a mean DpR of 0% (interquartile range: −16%, 10%) and a minimum DpR of −111%. The median period until maximum shrinkage was 12 weeks (±3.4).
Univariate and multivariate analyses of predictors of clinical outcome
For the group of FOLFIRI plus C-mab, univariate Cox regression analysis was used to assess the ability of peritoneum metastasis and DpR (≥30%) to predict PFS (Table 2). Univariate Cox regression analysis was used to assess the ability of sex, age, PS, and DpR (≥30%) to predict OS. In the multivariate Cox regression analysis, DpR (≥30%) was the strongest predictor of PFS. Age, PS, and DpR (≥30%) were the strongest predictors of OS (Figure 2).
On the other hand, for the group of FOLFIRI plus Bev, univariate Cox regression analysis was used to assess the ability of region of cancer, liver metastasis, lung metastasis to predict PFS. Univariate Cox regression analysis was used to assess the ability of liver metastasis, lymph node metastasis, and DpR (≥0%) to predict OS. In the multivariate Cox regression analysis, peritoneum metastasis and lymph node metastasis were predictors of PFS. Peritoneum metastasis and lymph node metastasis were the strongest predictors of OS.
Discussion
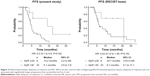
Generally, DpR is defined as the change in the sum of the longest diameters (LDs) of RECIST target lesions at the nadir in comparison with that at baseline. The CRYSTAL10 and OPUS11 trials were the first to provide evidence of a correlation between DpR and OS or post-progression survival. To our knowledge, this study is the first to investigate the relationship between DpR and clinical outcome in patients treated with second-line FOLFIRI plus C-mab. Our results show that a DpR of greater than or equal to 30% was associated with significantly longer OS and PFS when compared with a DpR of less than 30% in second-line FOLFIRI plus C-mab. However, when we also used the date of diagnosing RECIST-based progressive disease, DpR was not associated with significantly longer PFS like the FIRE-3 trial (Figure 3).
It is suggested that the clinical outcomes could be different when the RECIST standards of disease progress were chosen. When we give chemotherapy after primary treatment in our practice, we do it according to disease progress compared with before treatment, and if the tumor diameters increased by more than 20%. This is because there are few choices in patients with KRAS mutant tumors after primary treatment. These standards for disease progress were used in the SOFT study. Therefore, it is necessary to determine whether standards of the disease progression should change depending on the characteristics of the treatment drug and treatment line. For example, when a drug with a cytoreductive effect is used, such as C-mab, or when a patient has stable disease.
We also compared DpR with clinical outcomes of 70 FOLFIRI plus Bev continuation cases between the same periods of this study. When FOLFIRI plus C-mab is given to mCRC patients as second-line chemotherapy, these patients have rapid progression and they cannot reach third-line chemotherapy. We usually give FOLFIRI plus Bev for mCRC patients as second-line chemotherapy and leave an anti-EGFR inhibitor as third-line chemotherapy.
There was a minor correlation between DpR and clinical outcomes in patients administered FOLFIRI plus Bev. In the analysis of KRAS wild type patients only, there was a similar relationship between them (n=36, OS: r=-0.14, P=0.40; PFS: r=0.36, P=0.03) (Figure S1). Indeed, the biological effects of C-mab and Bev are different. It has been postulated that tumoral cavitation occurs through central necrosis of lesions after inhibition of angiogenesis, and is associated with a response to anti-angiogenic treatment.12 Tumor cavitation occurred in 19% of patients with non-small cell lung cancer treated with Bev, and this cavitation demonstrated three types of radiographic patterns.13 Evaluation of response based on three computed tomography criteria (tumor cavitation, ground-glass opacity component, and change in attenuation) in non-small cell lung cancer patients treated with Bev yielded a different result than that based on the traditional RECIST criteria.14 Conventional RECIST-based response assessment does not allow tumor progression by filling in of the cavity to be captured. Therefore, an alternative method of tumor measurement incorporating tumoral cavitation was proposed in 2009, and has been shown to alter response assessment and time-to-progression in a minority of patients.12 Laubender et al developed a World Health Organization-based tumor volume algorithm with good approximation to the true tumor volume using both the LD and the longest orthogonal diameter of the target lesion.15 Estimating volume based on the LD alone (RECIST-based volume) yields a tendency toward overestimating “true” volumes. Therefore, information on the longest orthogonal diameter is critical and the RECIST-based information is misleading. Volume-based values cover a wider range than LD-based assessments. The range of LD measurements corresponding to a given volume-based value is smaller than the range of volume based measurements corresponding to a given LD-based value.
The present study has some limitations. This was a retrospective study and the sample size was small. And there were differences in patient characteristics. As mentioned above, we give FOLFIRI plus C-mab to mCRC patients who have rapid progression and cannot reach third-line chemotherapy. Furthermore, patients in whom we expected tumor shrinkage tended to receive chemotherapy and C-mab, so there was selection bias in this study. Further study is needed to perform a sub-analysis of the relationship between DpR and clinical outcome using other biomarkers such as KRAS exon 3.4, NRAS, BRAF, and PIK3CA. Further research may improve the predictive accuracy of on-treatment markers, perhaps by implementing volumetric measurements and/or differentiating between organ metastases and lymph nodes. Careful validation is needed to determine this model’s potential in guiding individual clinical decision making in treating mCRC patients.
In conclusion, the present results indicate the potential of DpR as a new measure of efficacy in mCRC patients treated with second-line chemotherapy. FOLFIRI plus C-mab as second-line chemotherapy yielded a stronger correlation between DpR and clinical outcome.
Acknowledgment
This work was supported by a Grant-in-Aid for Scientific Research (Japan Society for the Promotion of Science) (grant number 24591988).
Disclosure
S Matsusaka: commercial research grant, Taiho Pharmaceutical Co., Ltd; E Shinozaki: honoraria from speakers bureau, Taiho Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co., Ltd., Yakult Honsha Co., Ltd., Bristol-Myers Squibb, Takeda Pharmaceutical Co., Ltd; N Mizunuma: commercial research grant, Taiho Pharmaceutical Co., Ltd., Chugai Pharmaceutical Co., Ltd., Yakult Honsha Co., Ltd., Bristol-Myers Squibb, Takeda Pharmaceutical Co., Ltd., Merck Serono Co., Ltd., ONO Pharmaceutical Co., Ltd., Bayer Yakuhin Co., Ltd., All remaining authors have declared no conflicts of interest.
References
Giantonio BJ, Catalano PJ, Meropol NJ, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;20;25(12):1539–1544. | ||
Grothey A, Sugrue MM, Purdie DM, et al. Bevacizumab beyond first progression is associated with prolonged overall survival in metastatic colorectal cancer: results from a large observational cohort study (BRiTE). J Clin Oncol. 2008;26(33):5326–5334. | ||
Bennouna J, Sastre J, Arnold D, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147) a randomized phase 3 trial. Lancet Oncol. 2013;14(1):29–37. | ||
Sobrero AF, Maurel J, Fehrenbacher L, et al. EPIC: Phase III Trial of Cetuximab Plus Irinotecan After Fluoropyrimidine and Oxaliplatin Failure in Patients With Metastatic Colorectal Cancer. J Clin Oncol. 2008;26(14):2311–2319. | ||
Peeters M, Price TJ, Cervantes A, et al. Randomized Phase III Study of Panitumumab With Fluorouracil, Leucovorin, and Irinotecan (FOLFIRI) Compared With FOLFIRI Alone As Second-Line Treatment in Patients With Metastatic Colorectal Cancer. J Clin Oncol. 2010;28(31):4706–4713. | ||
Hecht JR, Cohn A, Dakhil S, et al. SPIRITT (study 2006014): A randomized phase II study of FOLFIRI with either panitumumab or bevacizumab as second-line treatment in patients with wild-type KRAS metastatic colorectal cancer. J Clin Oncol. 2012;30(suppl 34):A454. | ||
Heinemann V, Fischer von Weikersthal L, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol. 2014;15(10):1065–1075. | ||
Mansmann U, Sartorius U, Laubender R, et al. Deepness of response: A quantitative analysis of its impact on post-progression survival time after first-line treatment in patients with mCRC. J Clin Oncol. 2013;30(Suppl 4):A427. | ||
Fukushima Y, Yanaka S, Murakami K, et al. [High-throughput screening method of KRAS mutations at codons 12 and 13 in formalin-fixed paraffin-embedded tissue specimens of metastatic colorectal cancer]. Gan To Kagaku Ryoho. 2011;38(11):1825–1835. Japanese. | ||
Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med. 2009;2;360(14):1408–1417. | ||
Bokemeyer C, Bondarenko I, Hartmann JT, et al. Efficacy according to biomarker status of cetuximab plus FOLFOX-4 as first-line treatment for metastatic colorectal cancer: the OPUS study. Ann Oncol. 2011;22(7):1535–1546. | ||
Crabb SJ, Patsios D, Sauerbrei E, et al. Tumor cavitation: impact on objective response evaluation in trials of angiogenesis inhibitors in non small-cell lung cancer. J Clin Oncol. 2009;27(3):404–410. | ||
Nishino M, Cryer SK, Okajima Y, et al. Tumoral cavitation in patients with non-small-cell lung cancer treated with antiangiogenic therapy using bevacizumab. Cancer Imaging. 2012;12:225–235. | ||
Lee HY, Lee KS, Hwang HS, et al. Molecularly targeted therapy using bevacizumab for non-small cell lung cancer: a pilot study for the new CT response criteria. Korean J Radiol. 2010;11(6):618–626. | ||
Laubender R, Schlichting M, Sartorius U, et al. Evaluating the agreement between the empirical volumes of tumor lesions and the estimated volumes of tumor lesions based on the longest diameter. J Clin Oncol. 2012;30(Suppl 4):A635. |
Supplementary material
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.