Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Adjunctive treatment with aripiprazole for risperidone-induced hyperprolactinemia
Authors Ranjbar F, Sadeghi-Bazargani H, Niari Khams P, Arfaie A, Salari A, Farahbakhsh M
Received 9 June 2014
Accepted for publication 8 August 2014
Published 2 March 2015 Volume 2015:11 Pages 549—555
DOI https://doi.org/10.2147/NDT.S69088
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Roger Pinder
Fatemeh Ranjbar,1 Homayoun Sadeghi-Bazargani,2,3 Parisa Niari Khams,1 Asghar Arfaie,1 Azim Salari,4 Mostafa Farahbakhsh1
1Clinical Psychiatry Research Center, Tabriz University of Medical Sciences, Tabriz, East Azerbaijan, Iran; 2Road Traffic Injury Research Center, Department of Statistics & Epidemiology, Tabriz University of Medical Sciences, Tabriz, Iran; 3World Health Organization Collaborating Center on Community Safety Promotion, Karolinska Institute, Stockholm, Sweden; 4Emam Khomeini Hospital, Naghadeh, West Azerbaijan, Iran
Background: Antipsychotics have been used for more than 50 years in the treatment of schizophrenia and many other psychiatric disorders. Prolactin levels usually increase in patients treated with risperidone. Aripiprazole, which has a unique effect as an antipsychotic, is a D2 receptor partial agonist. It is an atypical antipsychotic with limited extrapyramidal symptoms. Since it acts as an antagonist in hyperdopaminergic conditions and as an agonist in hypodopaminergic conditions, it does not have adverse effects on serum prolactin levels. The present study aimed to investigate the effect of aripiprazole on risperidone-induced hyperprolactinemia.
Methods: This before-and-after clinical trial was performed in 30 patients. Baseline prolactin levels were measured in all patients who were candidates for treatment with risperidone. In subjects with elevated serum prolactin, aripiprazole was added to their treatment. Serum prolactin levels were measured during the first week, second week, and monthly thereafter for at least 3 months or until prolactin levels became normal. The data were analyzed using Stata version 11 software. Survival analysis and McNemar’s test were also performed.
Results: The mean age of the participants was 30.8 years. Prolactin levels normalized in 23 (77%) participants during the study, and menstrual disturbances normalized in 25 (83.3%). Prolactin levels normalized in most patients between days 50 and 110. The median time to recovery based on normalization of prolactin was 84 days. Psychotic symptoms were present in 26 subjects at baseline, but in only two by the end of the study.
Conclusion: The results of this study confirm the effects of aripiprazole in reducing risperidone-induced hyperprolactinemia and its sequelae. Aripiprazole also led to significant improvements in psychotic symptoms when compared with those present prior to treatment with aripiprazole.
Keywords: hyperprolactinemia, aripiprazole, risperidone, psychotic disorder
Background
Antipsychotics have been used for more than 50 years in the treatment of schizophrenia and many other psychiatric disorders.1,2 Second-generation antipsychotics, in particular risperidone and clozapine, have revolutionized the treatment of schizophrenia. Risperidone is now commonly used as an atypical antipsychotic drug and has a high affinity for dopamine-D2 and 5-HT2 receptors. It is approved by the US Food and Drug Administration for the treatment of psychotic disorders. The extrapyramidal complications of risperidone are less than with the typical antipsychotics. Risperidone also reduces the likelihood of hospitalization.3,4
Prolactin levels increase in patients treated with risperidone, and this increase is higher than that seen with other second-generation antipsychotics.5–7 There is some evidence that this increase in prolactin levels depends on the dose of risperidone8 and is more common in women.5 An increase in prolactin levels may have short-term and long-term consequences, which can seriously affect quality of life. Menstrual disorders, galactorrhea, sexual dysfunction, gynecomastia, infertility, and reduced bone density are some of these complications. Recent investigations have shown that risperidone may even increase the risk of developing breast cancer. However, further investigations are required in this regard.9–12 In antipsychotic-induced hyperprolactinemia, high percentages of osteoporosis and osteopenia are seen in patients taking long-term treatment. Young women, in particular, are more vulnerable to loss of bone density and hypogonadism.13
Aripiprazole, which has a unique effect as an antipsychotic, is a D2 receptor partial agonist, a 5-HT1a partial agonist, and a 5-HT2a receptor antagonist. It is an atypical antipsychotic with limited extrapyramidal symptoms. It is effective in the treatment of the positive and negative symptoms of psychosis and similarly for mood symptoms. Since it acts as an antagonist in hyperdopaminergic conditions and as an agonist in hypodopaminergic conditions, it does not have adverse effects on serum prolactin levels.14 In a study conducted by Stroup et al, use of aripiprazole as a replacement for olanzapine, quetiapine, and risperidone reduced non-high-density lipoprotein, triglycerides, and body weight in patients.15 In a study by Byerly et al, adding aripiprazole to risperidone reduced prolactin levels in both men and women during the first week. The present study aimed to investigate the effect of aripiprazole in reducing risperidone-induced hyperprolactinemia.
Subjects and methods
Subjects
The study population included all female patients referred to the psychiatry clinic of Razi University Hospital in Tabriz during the years 2013 and 2014 and selected on the basis of inclusion and exclusion criteria. Forty-seven patients volunteered to participate in the study. All had normal baseline prolactin levels, but three dropped out of the study. Thirty of the subjects had developed elevated prolactin levels following 2 months of treatment with risperidone. All of the subjects with hyperprolactinemia reported menstrual cycle changes, including changes in volume and duration of menstruation, and the interval between cycles.
Design
This before-and-after clinical trial was performed in 30 patients. Inclusion criteria were: childbearing age; a diagnosis of schizophrenia, delusional disorder, or refractory obsessive compulsive disorder; suitability for treatment with risperidone; and ability to provide written informed consent. Exclusion criteria were: history of amenorrhea before receiving medication; lactation; pregnancy; renal failure; hypothyroidism; pituitary tumors; history of seizures; and being on antipsychotic drugs, methyldopa, levodopa, cimetidine, estrogen, or opiates.
Outcome
Baseline prolactin levels were measured in all patients who were candidates for treatment with risperidone. To reduce the possibility of a confounding effect of baseline prolactin levels and to improve the statistical power of the study for the given number of patients, only patients with normal baseline prolactin were enrolled. The patients continued treatment with risperidone for at least 2 months, and if they developed elevated serum prolactin, aripiprazole was added to their treatment. Serum prolactin levels were measured during the first week, second week, and monthly for at least 3 months or until prolactin levels decreased to normal. Fasting blood sampling was performed for all the participants up to 3 hours after waking up in the morning. Considering that the half-life of prolactin is 30 minutes and its secretion is strongly influenced by stress, patients were required to rest for half an hour in the laboratory before blood sampling. Necessary instructions were given in this regard including:
- Fasting for about 8 hours before blood sampling
- Avoiding breast stimulation, which may increase prolactin levels
- Fasting blood sampling to be performed up to 3 hours after awakening
- Resting for half an hour in the laboratory before blood sampling
- Avoiding sexual contact before the test
- Avoiding any stress and physical activity.
Since stimulation of the breast, for whatever reason, increases prolactin, necessary explanations were given in this regard and the importance of avoiding sexual contact before the test was emphasized. Blood sampling was carried out by experienced staff to minimize stress and avoid any effects on hormone levels. Different laboratories were used, so serum prolactin levels were measured by different electrochemiluminescence and immunoassay systems.
The doses of risperidone and aripiprazole were adjusted according to the patient’s response, which was evaluated by reduction in clinical signs of the primary disorder that was the indication for risperidone. The effect of aripiprazole was evaluated by the serum prolactin level and patient-reported improvement in menstrual disturbances.
The starting dose of aripiprazole was 5 mg, and if adverse effects developed, it was decreased to 2.5 mg (in two patients). The dose was increased every 2 weeks by telephone follow-up. The subjects were assessed for common side effects before and after treatment with aripiprazole.
Statistical analysis
The data were analyzed using Stata version 11 software (Statacorp LP, Whitehouse Station, TX, USA). Since the methods and normal ranges of the tests were different, the prolactin value was divided by the maximum value of the normal laboratory range threshold, and the result of it was used as the scale of prolactin level to be compared before and after the treatment in this study. A value >1 was considered abnormal. However, values >1 were included in the data analysis as an outcome measure to ensure comparability among patients. The following statistical methods were used:
- Survival analysis and plotting of Kaplan–Meier curves. Two survival outcomes were analyzed using this methodology; first, the length of time for normal prolactin levels to be reached in each patient who had hyperprolactinemia; and second, the length of time for the clinical symptoms of hyperprolactinemia to resolve after treatment.
- The natural logarithm of the prolactin level was calculated to normalize the data distribution.
- Longitudinal data analysis was also done to compare repeated measurements of the prolactin level scale. Considering the data distribution and that some data were missing, the Skillings–Mack test was used to analyze the data.
- McNemar’s test was used to assess changes in the status of categorical scaled variables, such as pre- and post-study effects.
Patients participated in this study voluntarily and were allowed to leave the study at any time. Written informed consent was obtained from all patients and their guardians. Ethical approval for the study was obtained from the Medical Ethics Committee of Tabriz University of Medical Sciences (5/4/7828) and the study is registered on the clinical trials website of the Islamic Republic of Iran (IRCT2013071822181N6).
Results
The mean (± standard deviation) age of the participants was 30.8±6.4 years. Eleven (36.6%) participants had academic education. Thirteen (43.3%) had no history of hospitalization. Twelve (40%) had been hospitalized once and five (16.6%) patients had been hospitalized more than once. The average weight of participants before the intervention was 62.9±8.3 kg and after the intervention was 64.8±9 kg. This change was not statistically significant.
The median and mean doses of risperidone were 2 mg/day and 2.5 mg/day, respectively. The maximum dose of risperidone was 6 mg/kg. The minimum starting dose of aripiprazole was 2.5 mg/day and the maximum dose was 25 mg/day (in some subjects).
Prolactin levels normalized in 23 subjects during the study. The change in repeat measurements of prolactin level over time was statistically significant using the Skillings–Mack test (P<0.05). The individual trend for normalization of prolactin in each sample is shown in Figure 1.
  | Figure 1 Individual trend for normalization of prolactin on adjunctive aripiprazole. |
All of the subjects with hyperprolactinemia reported menstrual cycle changes, including changes in the volume and duration of bleeding, and the interval between menstrual cycles. According to patient self-reporting, menstrual cycle changes normalized in 25 (83.3%) subjects during the study period. Prolactin normalized between days 50 and 110 in most patients. The median time to recovery based on normalization of prolactin levels and resolution of menstrual disturbances was 84 and 81 days, respectively. The first quartile of normalization of prolactin levels was 77 days and the third quartile was 106 days. The Kaplan–Meier survival curve for normalization of prolactin is shown in Figure 2.
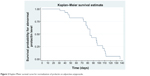  | Figure 2 Kaplan–Meier survival curve for normalization of prolactin on adjunctive aripiprazole. |
Two patients at the first follow-up and one patient at the third follow-up had prolactin levels more than 100 times the upper limit of the normal range (see Figure 3), so to compare changes, the natural logarithm of prolactin level was used instead of prolactin level to nonlinearly minimize the numbers. The declining prolactin level, data distribution, and means are shown in Figure 3, and indicate treatment efficacy.
According to the information supplied by the study participants, 97.7% had normal cholesterol levels at the beginning of the study (with the exception of one subject who reported abnormal levels). Triglyceride levels increased in one of the 30 subjects after the intervention. As shown in Table 1, two of the 30 patients had headaches before the start of the intervention and recovered by the end of the study, and two patients developed headaches after the intervention. Four patients had insomnia at the beginning of the study, two of whom recovered by the end of the study. Twenty-six patients had psychotic symptoms at baseline and this number dropped to two at the end. These changes were statistically significant. At baseline, nine patients complained of sexual problems, which decreased to five by the end of the study. However, this change was not statistically significant. Ten patients suffered from anxiety at the beginning of the study, but only eight did so by the end of the study, and this decrease was not statistically significant.
Discussion
Prolactin levels normalized in 23 subjects and menstrual disturbances resolved in 25 (83.3%) subjects during the study. The mean age of our study participants was 30.8 years, which is lower than the mean age of 48.3 years in a study reported by Chen et al.16 In terms of gender, all subjects were women of childbearing age. The only other study in which all participants were women was that reported by Yausi-Furukori et al,21 so selecting women of childbearing age distinguishes our study from most of the other studies. In the study by Chen et al all subjects were men, but from the standpoint of efficacy in decreasing prolactin levels, similar results were obtained, suggesting that aripiprazole reduces serum prolactin levels in both sexes.16
Our results showed that adding aripiprazole to risperidone improved serum prolactin levels in 23 of 30 subjects, and resulted in resolution of menstrual disturbances in 25 cases. This finding is consistent with other studies that support the addition of aripiprazole to risperidone.16–19 The mechanism of this decrease, as also discussed in the research by Kotorki et al can be explained as follows: when aripiprazole is added to risperidone, given the higher affinity of aripiprazole than risperidone for the D2 receptor,18 aripiprazole forms a stronger bond with this receptor, and in a hypodopaminergic environment induced by previous treatment with risperidone, acts as a dopamine agonist and reverses the process of prolactin production.20
In most individuals, normalization of serum prolactin occurred between days 50 and 110, and the median time to recovery was 84 days based on normalization of prolactin. In contrast, most patients in a study by Shores et al reached normal levels within the first 2 weeks,19 and in a study by Chen et al the time to recovery was reported to be about 4 weeks.16 Further, in a study by Lee et al published in 2013, the recovery time was reported to be 24 weeks.17 These different time frames for recovery are possibly due to differences in study populations and the speed of titration of aripiprazole.
Titration of aripiprazole in the present study was done monthly, with dose increases until normal prolactin levels were reached. The maximum dose in our study was 25 mg/day. This method of titration is similar to that used by Yausi-Furukori et al, however, in their study, the time taken for normalization of serum prolactin was not reported.21
Lee et al17 reported that adding aripiprazole to risperidone reduced extrapyramidal complications. However, in our study, although extrapyramidal complications were not investigated, a decrease in sensation of akathisia was reported by a small number of patients, but was not statistically significant.
According to the findings of Shah et al in 2012, individuals who received aripiprazole had fewer sexual problems than those taking risperidone.22 Sexual complaints decreased similarly in our study, albeit not significantly, which is not consistent with the findings of Chen et al who observed significant improvements in sexual problems after treatment with aripiprazole.16
Psychotic symptoms were present in 26 subjects at baseline, but in only two by the end of the study. This change was statistically significant. Given that all of the subjects received risperidone and the antipsychotic effect of aripiprazole is weak, this marked reduction in psychotic symptoms could be attributed to risperidone. No previous study has mentioned improvement of psychotic symptoms. Only Lee et al reported that adding aripiprazole to risperidone reduced negative symptoms in patients.17
This study has several limitations. The duration of effect of aripiprazole on risperidone-induced hyperprolactinemia is unknown, so further studies are needed in the future to clarify this issue. One of the methodological limitations of this study was the lack of a placebo control group, which should be considered in future studies. Our study was performed only in women of childbearing age to evaluate the risk of antipsychotic-induced hyperprolactinemia. There is some evidence suggesting that risperidone has an effect on prolactin levels in teenagers,23 so it is suggested that future studies be planned and implemented in specific age groups, such as children and teenagers, and also in men. Finally, our study did not investigate the cognitive effects of adding aripiprazole to risperidone, and this should also be considered in future research.
Conclusion
The results of this study confirm the potential effect of aripiprazole in reducing risperidone-induced hyperprolactinemia and its sequelae. Aripiprazole also led to significant improvements in psychotic symptoms. Our findings suggest that in patients who cannot substitute risperidone with clozapine or other antipsychotics that have no effect on serum prolactin, addition of aripiprazole to risperidone is a beneficial strategy which, in addition to decreasing risperidone-induced prolactin levels, improves psychosis and some of its symptoms.
Acknowledgments
This paper was prepared from a PhD thesis in psychiatry at the Tabriz University of Medical Sciences and sponsored by the Clinical Psychiatry Research Center at this university. The authors thank all the patients who volunteered to participate in this research. We are also grateful to the psychiatry faculty members at the Tabriz University of Medical Sciences, who helped us by collecting and introducing patients for this research.
Disclosure
The authors report no conflicts of interest in this work.
References
Guff DC. Risperidone. In: Schatzberg AF, Nemeroff CB, editors. Textbook of Psychopharmacology. 3th ed. Arlington, VA, USA: American Psychiatric Publishing; 2004. | ||
Litman RE, Su TP, Potter WZ, Hong WW, Pickar D. Idazoxan and response to typical neuroleptics in treatment-resistant schizophrenia. Comparison with the atypical neuroleptic, clozapine. Br J Psychiatry. 1996;168:571–579. | ||
Peuskens J. Risperidone in the treatment of patients with chronic schizophrenia: a multi-national, multi-centre, double-blind, parallel-group study versus haloperidol. Risperidone Study Group. Br J Psychiatry. 1995;166:712–726. | ||
Raja M. Pharmacotherapy update: risperidone in the treatment of schizophrenia. Clinical Medicine: Therapeutics. 2009;1:1199–1214. | ||
Petty RG. Prolactin and antipsychotic medications: mechanism of action. Schizophr Res. 1999;35:67–73. | ||
Tourrone P, Kapur S, Seeman MV, Flint AJ. Elevation of prolactin levels by atypical antipsychotics. Am J Psychiatry. 2002;159:133–135. | ||
Volavka J, Czobor P, Cooper TB, et al. Prolactin levels in schizophrenia and schizoaffective disorder patients treated with clozapine, olanzapine, risperidone, or haloperidol. J Clin Psychiatry. 2004;65:57–61. | ||
Kleinberg DL, Davis JM, de Coster RD, Van Baelen B, Brecher M. Prolactin levels and adverse events in patients treated with risperidone. J Clin Psychopharmacol. 1999;19:57–61. | ||
Bostwick JR, Guthrie SK, Ellingrod VL. Antipsychotic-induced hyperprolactinemia. Pharmacotherapy. 2009;29:64–73. | ||
Haddad PM, Wieck A. Antipsychotic-induced hyperprolactinaemia: mechanisms, clinical features and management. Drugs. 2004;64:2291–2314. | ||
Byerly MJ, Marcus RN, Tran QV, Eudicone JM, Whitehead R, Baker RA. Effects of aripiprazole on prolactin levels in subjects with schizophrenia during cross-titration with risperidone or olanzapine analysis of a randomized, open label study. Schizophr Res. 2009;107:218–222. | ||
Montejo M. Prolactin awareness: an essential consideration for physical health in schizophrenia. Eur Neuropsychopharmacol. 2008;18:108–114. | ||
O’Keane V. Antipsychotic-induced hyperprolactinemia and osteoporosis in the treatment of schizophrenia. J Psychopharmacol. 2008;22:70–75. | ||
Keck PE Jr, McElroy SL. Aripiprazole: a partial dopamine D2 receptor agonist antipsychotic. Expert Opin Investig Drugs. 2003;12:655–662. | ||
Stroup TS, McEvoy JP, Ring KD, et al. A randomized trial examining the effectiveness of switching from olanzapine, quetiapine, or risperidone to aripiprazole to reduce metabolic risk: comparison of antipsychotics for metabolic problems (CAMP). Am J Psychiatry. 2011;243:123–127. | ||
Chen CY, Lin TY, Wang CC, Shuai HA. Improvement of serum prolactin and sexual function after switching to aripiprazole from risperidone in schizophrenia: a case series. Psychiatry Clin Neurosci. 2011;65:99–97. | ||
Lee BJ, Lee SJ, Kim MK, et al. Effect of aripiprazole on cognitive function and hyperprolactinemia in patients with schizophrenia treated with risperidone. Clin Psychopharmacol Neurosci. 2013;11:60–66. | ||
Rainka MM, Capote HA, Ross CA, Gengo FM. Attenuation of risperidone-induced hyperprolactinemia with the addition of aripiprazole. J Clin Pharm Ther. 2009;34:595–598. | ||
Shores LE. Normalization of risperidone-induced hyperprolactinemia with the addition of aripiprazole. Psychiatry (Edgmont). 2005;2:42–45. | ||
Kotorki P, Pelka P, Leotsakou C, et al. Reversal of symptomatic antipsychotic-induced hyperprolactinemia with addition of aripiprazole. Ann Gen Psychiatry. 2010;9 Suppl 1:S164. | ||
Yasui-Furukori N, Furukori H, Sugawara N, Fujii A, Kaneko S. Dose-dependent effects of adjunctive treatment with aripiprazole on hyperprolactinemia induced by risperidone in female patients with schizophrenia. J Clin Psychopharmacol. 2010;30:596–599. | ||
Shah SK. A comparative study of sexual dysfunction in schizophrenia patients taking aripiprazole versus risperidone. Kathmandu Univ Med J (KUMJ). 2013;42:121–125. | ||
Margari L, Matera E, Craig F, et al. Tolerability and safety profile of risperidone in a sample of children and adolescents. Int Clin Psychopharmacol. 2013;28(4):177–183. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


