Back to Journals » Clinical Ophthalmology » Volume 8
Adjunctive therapy patterns in glaucoma patients using prostaglandin analogs
Authors Schmier J, Hulme-Lowe C, Covert D
Received 8 March 2014
Accepted for publication 29 April 2014
Published 10 June 2014 Volume 2014:8 Pages 1097—1104
DOI https://doi.org/10.2147/OPTH.S63760
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 6
Jordana K Schmier,1 Carolyn K Hulme-Lowe,1 David W Covert2
1Exponent, Alexandria, VA, USA; 2Alcon Research Ltd., Fort Worth, TX, USA
Purpose: To analyze patterns of use of adjunctive therapies among new initiators of topical prostaglandin analogs (PGAs) in a managed care population.
Methods: The study cohort included patients in a claims database who initiated PGA therapy between June 2007 and April 2011. Patients who had one or more adjunctive therapy prescriptions during 24 months of follow-up were included. Patterns of adjunctive therapy use were identified and compared between patients who had one or two fills of the initial adjunctive therapy and those who had three or more.
Results: There were 16,486 eligible beneficiaries. Of these, 5,933 (36%) had one or more adjunctive therapies within 24 months from the start of the PGA, 82% of whom started adjunctive therapy within 12 months. About 28% of patients started adjunctive therapy with a fixed-combination product; 45% of these patients started within the first 30 days. Overall, a large number of patients (42%) required adjunctive therapy within 30 days. Twenty-five percent of patients had only one or two prescriptions of their initial adjunctive therapy; of these patients, 74% discontinued adjunctive therapy altogether.
Conclusion: Approximately 30% of patients starting glaucoma therapy will require adjunctive therapy within 1 year, and many receive a fixed-combination product as initial adjunctive therapy shortly after starting glaucoma therapy. This suggests a prescribing trend toward earlier, more aggressive drug therapy to control pressure and minimize disease progression. We found that compliance with adjunctive therapy continues to be a problem for patients, which could be attributed to a number of treatment burden and economic factors.
Keywords: costs and cost analysis, drug therapy, combination, polypharmacy
Introduction
The benefits of achieving a low target intraocular pressure (IOP) in primary open-angle glaucoma (POAG) and ocular hypertension are well recognized. When acceptable IOP levels are not achieved with a single drug, adjunctive therapy with complementary mechanisms of action is recommended. The Ocular Hypertension Treatment Study (OHTS) found that, in eyes without significant optic nerve damage and at risk of developing glaucoma, more than 40% of patients needed additional medication within 5 years after starting treatment to reach a modest reduction in IOP of 20% or more long-term.1 As many as 75% of patients with POAG may require adjunctive therapy within 24 months of starting glaucoma therapy in order to achieve the target pressure.2 The Advanced Glaucoma Intervention Study (AGIS) found that, in patients with glaucoma, the number of patients requiring more than one drug might be as high as 80% when the disease is more severe.3 The introduction of adjunctive therapies to a treatment regimen multiplies the negative influences on adherence (ie, complexity of regimen, likelihood of adverse events, increased preservative load).4–11
Initial therapy for POAG and ocular hypertension is typically with a prostaglandin analog in the US. Outside the US, a beta-blocker is still frequently used as first-line therapy due to cost.12 When a prostaglandin analog is insufficient to control pressure, there are many types of adjunctive therapies to add, including selective and nonselective beta-blockers, alpha-agonists, and carbonic anhydrase inhibitors (CAIs), as well as lesser-used therapies, such as miotics. There are also fixed combinations available that include a nonselective beta-blocker when more than one adjunctive therapy is needed to control IOP. A fixed combination of an alpha-agonist and CAI is also now available for patients with a contraindication to a nonselective beta-blocker.
The use of a fixed-combination drug provides the opportunity to maximize pressure reduction by combining two complementary mechanisms of action in one bottle while minimizing the complexity of the treatment regimen. There is published evidence that multiple drops can be challenging to administer without assistance and there is also the increased risk of contamination from patients inadvertently touching multiple bottles to the eye.13–15 Additionally, as topical medications are applied frequently and over a long period of time, preservative toxicity to the ocular surface becomes an important factor for a chronic disease such as glaucoma.16–18 Previous studies suggest that the use of fixed-combination products for control of IOP has increased significantly over the past decade.7–9 This current study adds to this body of evidence by looking at more recent trends in glaucoma prescription use and, in particular, at the use of fixed-combination products in the treatment regimen.
Methods
The patients included in this retrospective cohort analysis were receiving medical and prescription benefits and were included in the 2007–2012 MarketScan® Commercial Claims and Encounters and Medicare Supplemental databases. The Commercial Claims and Encounters database covers more than 300 million lives and includes 12 health plans and approximately 100 employers and includes both employees and dependents (personal communication February 2013). The Medicare Supplemental and Coordination of Benefits database covers more than 2.5 million lives and includes patients 65 years and older with employer-paid or Medicare Part C coverage. Only services covered 100% by Medicare Part A or B are excluded. All data were de-identified in accordance with Protected Health Information standards under the Health Information Portability and Accountability Act so that no individually identifiable information was included in the study database. Therefore, review by an institutional review board was not required.
The study cohort included patients who first initiated therapy with one of three ophthalmic prostaglandin analogs (bimatoprost, latanoprost, or benzalkonium chloride (BAK)-free travoprost) between April 1, 2007 and April 30, 2011. To qualify, patients had to have 4 months of prior claims data in which there were no glaucoma therapy claims of any class and no claims for POAG (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 365.11).19 The index date was defined as the first date on which a prostaglandin analog was filled. Glaucoma therapy claims were defined unique product identifiers for human drugs required as part of the Food and Drug Administration’s listing process. Patients with two prostaglandin scripts, whether the same or different medications, on the index date were excluded, as it is unclear whether these were errors or drug trials. The study population was further defined by requiring patients to have at least 24 months of use of prostaglandin analogs following the index date (initial prostaglandin fill). This was operationalized as having at least one prescription for an ophthalmic prostaglandin analog during months 20–24 of the follow-up period; this could be the same medication as at the index date or a different prostaglandin. Patients were also required to be enrolled for 12 months following the first prescription for an adjunctive therapy. In some cases, where patients began adjunctive therapy more than 12 months after the index date, this extended beyond the original 24 months of continuous enrollment required; these patients were required to have additional follow-up beyond the 24 months. Patients with two adjunctive therapy prescriptions on their first date of adjunctive therapy were also excluded, as it was unclear how to classify these patients. Patients who did not meet these requirements (sufficient prior claims data, repeat use of a prostaglandin, use of one or more adjunctive therapies, sufficient follow-up after initiating adjunctive therapy) were excluded from the study database. Adjunctive medications were described by type (fixed combinations, beta-blockers, alpha-agonists, CAIs, plus other).
Participants were characterized in terms of available demographic characteristics (age and sex). Given previous evidence of patterns of discontinuation with nonselective beta-blockers,20 patients were categorized by whether their initial adjunctive therapy was a nonselective beta-blocker (as part of a fixed combination or as a single agent) or another treatment (alpha-agonist, CAI, or other). Further, patients were classified based on whether they exhibited short-term use of the initial adjunctive therapy, defined as one or two prescriptions filled versus three or more. The adjunctive therapies, if any, following discontinuation of the first adjunctive agent were identified. Mean number of days to initiation of adjunctive therapy was calculated for each cohort; the proportion of patients with an initial adjunctive therapy in prespecified time periods was also calculated. The annual rate of surgical procedures for glaucoma (identified by Current Procedural Terminology (CPT®) codes 68566, 66170, 66172, 66180, 66185, 66625, 66630, 66710, 66711, 66761, and 66762) was also calculated. Statistical comparisons were conducted using Stata software (v 12.1; StataCorp LP, College Station, TX, USA).
Results
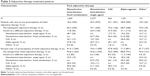
To provide context, existing studies on adjunctive therapy use were consulted. A review of the literature7–9 demonstrates a trend toward increased use of fixed-combination therapies as the first-line adjunctive therapy over time, with a corresponding decrease in the use of most single-agent drugs. These previously published studies used the same inclusion criteria and identified patients with a prescription for a topical prostaglandin analog who had no glaucoma therapy claims in the 6 months prior and had at least 12 months of data available after the initial prostaglandin analog claim. Thus, these analyses are comparable to each other and the present study, as shown in Figure 1.
  | Figure 1 Published estimates of adjunctive therapy use. |
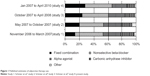
Figure 2 shows the patient identification process for this analysis. In the present analysis, there were 16,486 beneficiaries with at least one prostaglandin analog prescription who met all requirements for eligibility. Table 1 shows that 5,933 (36%) had one or more pre-specified adjunctive therapies within 24 months from the start of the prostaglandin analog and had 12 months of follow-up available after the start of adjunctive therapy. For two-thirds of these patients (n=3,927), their initial adjunctive therapy was a nonselective beta-blocker, either alone (n=2,277) or as part of a fixed combination (n=1,650). The average age in all groups was just less than 70 years, and 51% of the patients were women.
  | Figure 2 Patient identification process. |
  | Table 1 Demographic characteristics |
Among patients who required adjunctive therapy, 25% had only one or two prescriptions of their initial adjunctive therapy. Of these patients, 74% did not have additional prescriptions for adjunctive therapies during the observation year, ie, for 12 months following the start of their adjunctive therapy (see Table 2). This ranged from 69% of patients with one or two prescriptions for an alpha-agonist to 82% of patients starting with a fixed-combination beta-blocker. Two of the largest shifts observed were patients who had one or two prescriptions for a fixed-combination beta-blocker switching to a single-agent beta-blocker, and vice versa (48.1% and 62.7%, respectively).
Among patients who had three or more prescriptions of their initial adjunctive therapy (75%), the vast majority (overall 93%, ranging from 89%–94% of patients by adjunctive therapy) continued long-term use of their initial therapy. For the 6%–11% who had a different adjunctive therapy for the fourth prescription, there was a wide range of agents used, with no clear pattern to suggest what was used next.
Time to initiating adjunctive therapies is shown in Table 3. Time to first adjunctive therapy was highest for patients starting adjunctive therapy with CAIs (mean 190 days) and lowest for those starting with an “other” medication (mean 63 days). However, the standard deviation was high for all groups. These are further broken down into categories that represent both data-driven and clinically meaningful time points. First, the proportions of patients who had a prescription for an adjunctive therapy on the same day (day 0) as their index prostaglandin analog prescription are shown. This varies from 25% for alpha-agonists to 44% for other medications. Across all therapies, this represents 30% of the patients identified in the study. The rate of starting adjunctive therapies on days 1–30 is much lower, at 12%, and the total for the first month is a notable 42%. The next category captures adjunctive therapies filled in months 2–6 after the index prostaglandin analog and includes 28% of adjunctive therapy start dates. The remaining categories for initiating adjunctive therapy are 7–12 months and greater than 12 months, and ranged from 12%–18% of adjunctive therapy start dates.
The rate of surgical procedures for glaucoma, not shown here, was extremely low (ie, less than 0.001 annually per person during the observation period). Thus, the rate of surgeries was not a significant factor in this study, nor were there enough observations to compare across adjunctive therapy groups.
Discussion
In this analysis, treatment patterns were examined for patients based on their first adjunctive therapy initiated within 24 months after receiving an initial prescription for a prostaglandin analog for glaucoma. As shown in Figure 1, fixed combinations are being increasingly used as the first-line adjunctive therapy, in nearly 30% of glaucoma cases. This suggests a trend by providers toward earlier, more aggressive use of drug therapy to control pressure and prevent disease progression. Additionally, close to one-third of all adjunctive therapy prescriptions were filled on the same date as their first prostaglandin analog prescription. Same-day intervention of a fixed combination with a prostaglandin analog would be indicative of later-stage disease diagnosis as the patient’s first diagnosis. The decision to provide a fixed-combination therapy initially versus an unfixed combination has been explored, with a recent meta-analysis suggesting lower rates of hyperemia with fixed combinations compared to either unfixed combinations or prostaglandin analog monotherapy.21 Visual-field loss may already be present and be the reason for the patient seeking diagnostic services and treatment from a provider. Interestingly, the rate of surgical interventions was very low. We did not compare rate of surgical procedures by time to initiating adjunctive therapy; had the counts been higher, we would have considered such an analysis to identify whether starting adjunctive therapy earlier was indicative of more advanced disease.
In Table 2, we show that 25% of the patients had only one or two fills of their initial adjunctive therapy and often discontinued therapy altogether; only 26% of these patients continued therapy with a different agent. Of note, in the group of patients with only one or two fills of their initial adjunctive prescription, 76% of those patients that started with a nonselective beta-blocker (either single agent or fixed combination) discontinued all adjunctive therapy. Use of a nonselective beta-blocker is contraindicated for patients with a diagnosis of cardiovascular and/or respiratory disease.22–25 We found that 15% of the patients in the present study had a diagnosis for cardiovascular disease and 10% had a diagnosis for respiratory disease, but this could not be attributed directly to their discontinuation of adjunctive therapy.
Although discontinuation of nonselective beta-blockers did not appear to be linked to cardiovascular or respiratory care, patients could have described subclinical conditions to their ophthalmologists, which might have altered treatment patterns and possibly have led someone to switch from a fixed-combination or single-agent nonselective beta-blocker to adjunctive therapy without a nonselective beta-blocker. Still, the high rate of discontinuation of the adjunctive therapy rather than a switch to a different therapy cannot be explained given that these patients continued to use their primary prostaglandin analog therapy.
As with any claims database analysis, there are certain limitations that must be acknowledged. The use of a large claims database offers an important strength in terms of sample size but shortcomings remain. We cannot tell to what extent ‘days to supply’ guidelines, which may differ across patients and are not documented in the database, may influence refill patterns. Also, the patient population in any given database may not match the general population of patients with the condition in question, although, in this analysis, the age and sex of the population reflect that of the general glaucoma population.26 Other characteristics, such as race, educational status, central corneal thickness, or self-reported health status, among others, are unknown. Although glaucoma is typically bilateral, the American Academy of Ophthalmology’s guidelines suggest that eyes may respond to different medications.27 Therefore, we cannot rule out the possibility that what we identify as adjunctive therapy might not, instead be a different treatment for the fellow eye. The population of prescribers may not accurately reflect national patterns, which could affect generalizability. Most claims databases have little or no data on the characteristics of prescribers, but as the data were from a large managed care organization, it is likely that there is a wide distribution of prescribers and practices. By their nature, claims databases only provide information on people with some type of insurance coverage, and those with coverage may be more likely to seek out and adhere to treatment. Finally, claims databases may contain coding biases or errors, although there is no reason to believe that these errors would be different across treatments; in addition, the claims in this database were reviewed and adjudicated before the database was prepared for this analysis.
The methodology for patient selection in this study is also subject to certain limitations. The study attempted to identify only patients who were new to therapy by requiring 4 months of glaucoma-free claims prior to the first prostaglandin analog prescription. However, there is no way to account for product samples, which one study identified as being received by 20% of patients,6 and which could translate into patients who were already taking prostaglandin analogs before our study identified them or continuing on adjunctive therapies while appearing not to have refilled them. However, since we also required that patients had no glaucoma diagnosis in the four months prior to the index date, the likelihood of them having received glaucoma therapies prior to their index date is low. Also, based on this study methodology, patients could have had poor adherence but still have been included; patients in the cohort analysis were required to have a minimum of two prostaglandin analog prescriptions filled during the 24-month follow-up period, but no attempt was made to assess medication possession ratio. Interestingly, research suggests that patients who use both an adjunctive therapy and a prostaglandin analog may be more compliant than those without adjunctive therapy, although compliance at 12 months was still only about 60% in the relevant study.28 However, other studies report that dosing errors are more common with adjunctive therapy29 and that time between refills increases when adjunctive therapy is initiated.30
This leaves the question as to why so many patients with glaucoma maintain prostaglandin use but discontinue adjunctive therapies when there is no obvious evidence of adverse events or surgical intervention contributing to the answer. Many studies31–37 have evaluated compliance with glaucoma medications, which consistently report, much like in other therapeutic areas, that compliance decreases as regimens become more complicated. Patients may decide that their adjunctive therapies are not important enough to use regularly and physicians may not realize that patients are not using them as prescribed. Future studies that include analysis of a full electronic medical record so that physician notes can be reviewed may answer some of these questions.
Conclusion
This analysis of adjunctive therapy use patterns in POAG patients shows that these drugs are being prescribed early in the timeline of the patient’s treatment. In light of trends across multiple studies, this suggests a prescribing trend towards earlier, more aggressive drug therapy for POAG. Related topics, such as the high rate of discontinuation from adjunctive therapies, could be explored through further analysis given additional robust data.
Author contribution
All authors participated in the development of the paper, with JKS and DWC leading study design, CKH-L and JKS focusing on the analysis, DWC and JKS developing an initial draft, and CKH-L providing review and comment. All authors critically revised and approved the final version.
Disclosure
This study was funded by a grant from Alcon Research Ltd., to Exponent. One author, DWC, is an employee of Alcon, while two authors (JKS, CKH-L) are Exponent employees. The authors report no other conflicts of interest in this work.
References
Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713; discussion 829–830. | ||
Lichter PR, Musch DC, Gillespie BW, et al; CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943–1953. | ||
[No authors listed]. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol. 2000;130(4):429–440. | ||
Konstas AG, Maskaleris G, Gratsonidis S, Sardelli C. Compliance and viewpoint of glaucoma patients in Greece. Eye (Lond). 2000;14 Pt 5: 752–756. | ||
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB. Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm. 2009;15(9):728–740. | ||
Friedman DS, Quigley HA, Gelb L, et al. Using pharmacy claims data to study adherence to glaucoma medications: methodology and findings of the Glaucoma Adherence and Persistency Study (GAPS). Invest Ophthalmol Vis Sci. 2007;48(11):5052–5057. | ||
Schmier JK, Covert DW, Robin AL. First-year treatment patterns among new initiators of topical prostaglandin analogs. Curr Med Res Opin. 2009;25(4):851–858. | ||
Schmier JK, Covert DW, Robin AL. First-year treatment costs among new initiators of topical prostaglandin analogs. Clin Ophthalmol. 2009; 3:637–644. | ||
Schmier JK, Covert DW, Robin AL. First-year treatment costs among new initiators of topical prostaglandin analog identified from November 2007 through April 2008. Curr Med Res Opin. 2010; 26(12):2769–2777. | ||
Schmier JK, Lau EC, Covert DW. Two-year treatment patterns and costs in glaucoma patients initiating treatment with prostaglandin analogs. Clin Ophthalmol. 2010;4:1137–1143. | ||
Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008; 115(8):1320–1327. | ||
Holló G, Thelen U, Teus MA, et al. Long-term outcomes of prostaglandin analog versus timolol maleate in ocular hypertensive or primary open-angle glaucoma patients in Europe. J Ocul Pharmacol Ther. 2011; 27(5):493–498. | ||
Hennessy AL, Katz J, Covert D, et al. A video study of drop instillation in both glaucoma and retina patients with visual impairment. Am J Ophthalmol. 2011;152(6):982–988. | ||
Hennessy AL, Katz J, Covert D, Protzko C, Robin AL. Videotaped evaluation of eyedrop instillation in glaucoma patients with visual impairment or moderate to severe visual field loss. Ophthalmology. 2010;117(12):2345–2352. | ||
Stone JL, Robin AL, Novack GD, Covert DW, Cagle GD. An objective evaluation of eyedrop instillation in patients with glaucoma. Arch Ophthalmol. 2009;127(6):732–736. | ||
Valente C, Iester M. Impact of glaucoma medication on ocular tissue. Expert Rev Ophthalmol. 2010;5(3):405–412. | ||
De Saint Jean M, Brignole F, Bringuier AF, Bauchet A, Feldmann G, Baudouin C. Effects of benzalkonium chloride on growth and survival of Chang conjunctival cells. Invest Ophthalmol Vis Sci. 1999;40(3): 619–630. | ||
Pisella PJ, Fillacier K, Elena PP, Debbasch C, Baudouin C. Comparison of the effects of preserved and unpreserved formulations of timolol on the ocular surface of albino rabbits. Ophthalmic Res. 2000;32(1):3–8. | ||
National Center of Health Statistics. ICD-9-CM Index to Diseases and Injuries Addenda. 2011. | ||
Schmier JK, Covert DW, Lau EC. Medical service encounters and payments associated with topical adjunctive therapy use of timolol for glaucoma. Clin Drug Investig. 2012;32(12):835–842. | ||
Quaranta L, Biagioli E, Riva I, et al. Prostaglandin analogs and timolol-fixed versus unfixed combinations or monotherapy for open-angle glaucoma: a systematic review and meta-analysis. J Ocul Pharmacol Ther. 2013;29(4):382–389. | ||
Houde M, Castilloux AM, Tingey D, Assalian A, LeLorier J. Prescription of topical antiglaucoma agents for patients with contraindications to beta-blockers. Can J Ophthalmol. 2003;38(6):469–475. | ||
Vinker S, Kaiserman I, Waitman DA, Blackman S, Kitai E. Prescription of ocular beta-blockers in patients with obstructive pulmonary disease: does a central electronic medical record make a difference? Clin Drug Investig. 2006;26(9):495–500. | ||
Chen YF, Avery AJ, Neil KE, Johnson C, Dewey ME, Stockley IH. Incidence and possible causes of prescribing potentially hazardous/contraindicated drug combinations in general practice. Drug Saf. 2005;28(1):67–80. | ||
Kaiserman I, Fendyur A, Vinker S. Topical beta blockers in asthmatic patients-is it safe? Curr Eye Res. 2009;34(7):517–522. | ||
Friedman DS, Wolfs RC, O’Colmain BJ, et al; Eye Diseases Prevalence Research Group. Prevalence of open-angle glaucoma among adults in the United States. Arch Ophthalmol. 2004;122(4):532–538. | ||
Preferred Practice Pattern. Primary Open Angle Glaucoma. San Francisco, CA: American Academy of Ophthalmology; 2010. Available from: http://one.aao.org/Assets/56c908e3-a939-45ea-b12b-8fe609f547b0/634965436587800000/primary-open-angle-glaucoma-pdf. Accessed May 12, 2014. | ||
Iskedjian M, Covert DW, Walker JH. Persistence with prostaglandin agonist use with and without adjunctive therapy for glaucoma patients: a Canadian population-based analysis. Patient. 2011;4(2):133–141. | ||
Robin AL, Novack GD, Covert DW, Crockett RS, Marcic TS. Adherence in glaucoma: objective measurements of once-daily and adjunctive medication use. Am J Ophthalmol. 2007;144(4):533–540. | ||
Robin AL, Covert D. Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology. 2005;112(5):863–868. | ||
Robin A, Grover DS. Compliance and adherence in glaucoma management. Indian J Ophthalmol. 2011;59 Suppl:S93–S96. | ||
Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology. 2009;116(11 Suppl):S30–S36. | ||
Robin AL, Novack GD, Covert DW, Crockett RS, Marcic TS. Adherence in glaucoma: objective measurements of once-daily and adjunctive medication use. Am J Ophthalmol. 2007;144(4):533–540. | ||
Sleath B, Robin AL, Covert D, Byrd JE, Tudor G, Svarstad B. Patient-reported behavior and problems in using glaucoma medications. Ophthalmology. 2006;113(3):431–436. | ||
Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112(6):953–961. | ||
Robin AL, Covert D. Does adjunctive glaucoma therapy affect adherence to the initial primary therapy? Ophthalmology. 2005;112(5): 863–868. | ||
Tsai JC, McClure CA, Ramos SE, Schlundt DG, Pichert JW. Compliance barriers in glaucoma: a systematic classification. J Glaucoma. 2003;12(5):393–398. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.