Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
A retrospective study to assess resource utilization in patients with cervical dystonia in the United Kingdom
Authors Raluy-Callado M, Gabriel S, Dinet J , Wang M, Wasiak R
Received 3 December 2014
Accepted for publication 31 January 2015
Published 9 March 2015 Volume 2015:11 Pages 647—655
DOI https://doi.org/10.2147/NDT.S78618
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Mireia Raluy-Callado,1 Sylvie Gabriel,2 Jérôme Dinet,2 Meng Wang,1 Radek Wasiak1
1Retrospective Observational Studies, Evidera, London, UK; 2Ipsen Pharma, Boulogne-Billancourt, France
Purpose: Cervical dystonia (CD) is a hypertonic condition caused by damage to the central nervous system. Very few studies have assessed the overall economic burden of the disease. The objective of this study was to describe the utilization of health care resources of patients with CD in the UK primary care setting, using a large population-based database.
Patients and methods: Adults with a first diagnosis of CD between January 1, 2007 and January 31, 2011, who were registered to a general practitioner (GP) practice contributing to The Health Improvement Network (THIN), were included. Sociodemographic and clinical characteristics were assessed at the time of diagnosis. Health care resource utilization and pharmacological treatment were investigated at the end of the first and second year after diagnosis.
Results: Overall, 4,024 newly diagnosed patients with CD were identified, with average age at diagnosis of 45 years old; 65.3% were female. Depression in the year prior to diagnosis was the most common comorbidity. Primary care utilization was high in the first year, with 99.2% of patients visiting their GP (on average 6.2 times), and 43% visiting a nurse (on average 2.5 times). Patients were most commonly referred to an orthopedic surgeon, and 15.9% reported at least one physiotherapy visit. In the second year, utilization was similar. Prescriptions of at least one of the investigated treatments were found in 82.0% and 45.3%, in the first and second year, respectively.
Conclusion: Findings suggest a high number of new CD cases are being identified in primary care, but not all will be referred to secondary care. Health care resource utilization was compared with that of all patients registered in THIN, which is representative of the UK, and the adjusted usage of primary care resources was found to be similar to that of the THIN population.
Keywords: primary care, health care utilization
Introduction
Dystonia is a hypertonic condition caused by damage to the central nervous system, which is associated with pulling and stiffness of muscles. There are several different forms of dystonia, which may affect only one muscle, groups of muscles, or muscles throughout the body. Cervical dystonia (CD), also called spasmodic torticollis, is classified as a focal dystonia since it is localized to a specific part of the body, and is the most common adult-onset dystonia. It is characterized by involuntary contractions of the cervical muscles that result in abnormal, sustained, and painful postures of the head, neck, and shoulders.1,2 The prevalence rate of CD ranges from 57.0 to 88.6 cases per one million in Europe and the USA, respectively, although in most studies, prevalence rates were based on relatively few cases, and hence estimates had wide confidence intervals (CIs). In the UK, the prevalence of CD has been estimated to be between 59 and 61 cases per million.3,4 Female predominance in CD has been noted in a series of studies.4–8 It is believed that the prevalence of CD is underreported due to the numbers of patients either not seeking medical treatment, being misdiagnosed, or being diagnosed late – only after the disease has become disabling.2,3
The onset of CD may be acute and painful or insidious and painless. Symptoms develop gradually over a period of time, with the intensity of the disease progressively worsening over the first 5 years.9,10 The rate of progression from symptom onset to difficulties in activities of daily living and disability can range from rapid development over days or weeks to a gradual progression over several years. Spontaneous remission of CD occurs in 12% to 20% of cases but is frequently only temporary.11 For most patients, CD is a chronic condition that stabilizes after the first 5 years. Spread to other segments of the body may also occur.
The management of CD is primarily symptomatic, designed to improve posture and function and to relieve associated pain.12 Chemodenervation with botulinum neurotoxin (BoNT) is established as the treatment of choice for adult-onset CD.13,14 Other oral medications, including anticholinergic agents, dopamine receptor antagonists, and gamma aminobutyric acid (GABA)-mimetic agents are also used in the treatment of CD,12 but treatment success with the use of these agents is limited and associated with a number of undesired adverse effects.15,16 Physical therapy is frequently combined with pharmacologic treatment to improve the benefit of medical interventions and prevent permanent muscle contracture.17 For patients whose symptoms are not alleviated by pharmacologic treatment, or who are refractory to pharmacologic treatment, surgical interventions may be an option. These include peripheral surgical denervation, selective dorsal ramistecomy, bilateral pallidotomy, or globus pallidus deep brain stimulation (which involves sending controlled amounts of electricity to the region in the brain that controls movement).18,19
Published cost studies for CD have focused only on the costs of specific treatments and, more recently, on the cost of treating CD with BoNT type A (BoNT-A).20,21 To date, very few studies have assessed the overall economic burden of the disease. In France, the annual cost of treating CD for patients who required BoNT-A injections in a neurological practice was estimated at, on average, €1,198 (2010), which included pharmaceutical costs of the BoNT-A injections and other medications, salaries, and conditioning and injection equipment. Differences in costs across patients were explained by the frequency of BoNT-A administration and duration of effect.22 However, at the present time, there are no other European studies that have estimated the overall economic burden of CD, including the UK.
The primary objective of this study was to describe the utilization of health care resources of patients with CD in the primary care UK setting, using a large population-based database. Both health care resource utilization and frequency of prescriptions by the general practitioner (GP) of the most common pharmacological treatments during the first and second year after diagnosis were assessed. Additional data variables described in the study included the sociodemographic and clinical characteristics of patients newly diagnosed with CD.
Material and methods
This retrospective study was conducted using data from individuals registered to a GP practice contributing to The Health Improvement Network (THIN) database. THIN database includes primary care records from 532 general practices representative of the UK population, with 3.7 million registered patients as of the end of September 2011.23 Available records include anonymized sociodemographic data, medical signs, symptoms and diagnoses described using Read codes (a standardized clinical coding system used by GPs in the UK), diagnostic and laboratory tests, referrals, and prescriptions of any medications issued by the GP.
Inclusion and exclusion criteria
This study included adults aged 18 years old and above at the time of first diagnosis of CD (index date) between January 1, 2007 and January 31, 2011. The diagnosis was identified by a single Read code – “F138200: spasmodic torticollis”; no other codes with the specific term “cervical dystonia” existed. All the available patient data up to January 31, 2013 was extracted. To ensure only newly diagnosed cases were captured, patients were excluded if they were first diagnosed within 6 months of registering with the GP practice.
The study time frame included patient records from 12 months prior to index date (baseline period) until end of follow up, which was defined as death, transfer out of the practice, or last data collection at the practice. Patients were required to have a minimum of 24 months of follow up after diagnosis so that resources could be investigated at two cross-sectional time points after diagnosis: at 12 and 24 months. Univariate tests were used to compare age, sex, and presence of comorbidities in patients with and without at least 24 months of follow up, to ensure no bias in the selection of the study population was introduced.
Statistical analysis
Sociodemographic and clinical characteristics of patients with CD were assessed at the time of diagnosis in the baseline period. These included age, sex, socioeconomic status, body mass index (BMI), smoking status, and the presence of the following comorbid conditions: stroke, multiple sclerosis, spinal cord injury, acquired brain injury, depression, and anxiety/sleep problems in the last 12 months.
Health care resource utilization and pharmacological treatment were investigated at the end of the first year and at the end of second year after diagnosis. Primary care resources investigation included GP visits and nurse visits at the GP practice. Some elements of the secondary care available were referrals to specialists, all-cause hospital admissions, and physical therapy.
Pharmacological treatments for CD that could be prescribed by the primary care GPs were the only information available, and this was investigated.12 Multilex codes for anticholinergic agents, muscle relaxants, pain medication, antiepileptics, dopamine receptor antagonists, and beta-blockers were used to identify pharmacological use. Information related to chemodenervation with BoNT was also investigated. However, in the UK this treatment is prescribed and administered directly in the secondary care setting. Thus, prescription information was not available in THIN, but instead, Read codes in the medical records were examined for information fed back from the specialist.
For continuous variables, the distribution of each of the study variables was summarized in terms of the mean, standard deviation (SD), median, and range of values. For categorical variables, the number and proportion at each level of the variable, with 95% confidence intervals (CI) around the proportion, were reported. The number and percentage of missing values, as applicable, were reported for each variable.
All analyses were conducted using commercially available statistical software (SAS version 9.2; SAS Institute Inc., Cary, NC, USA). The study was approved by the international Scientific Review Committee (SRC) to ensure appropriate analysis and interpretation of the data (SRC protocol 13-074).
Results
Overall, 6,352 patients had their first Read code for CD recorded between January 1, 2007 and January 31, 2011 (Figure 1). Patients were excluded for the following reasons: aged younger than 18 years old (n=1,068), less than 6 months between registration and index date (n=576), and less than 24 months of follow up after index date (n=684). Reasons for having less than 24 months follow up included: 37 patients who had died, 408 who had transferred out of the GP practice and the remaining 239 were enrolled in a practice for which the last data collection was earlier than January 31, 2013.
  | Figure 1 Sample selection flow chart. |
When comparing patients with at least 24 months of follow up and those with less than 24 months follow up, the only investigated characteristic that was significantly different between the two groups was age, as patients with less than 24 months of follow up were younger on average (mean age 41.3 vs 45.0) (P<0.0001). This could indicate higher residence mobility in younger generations, which was considered unrelated to the study outcomes, so the subgroup of patients with at least 24 months of follow up was considered suitable for the analysis of this study.
The CD population for this study included 4,024 patients across 4 years and 1 month, with about 1,000 new cases diagnosed per year across the study period.
Baseline characteristics
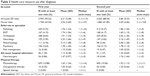
The average age at diagnosis of CD was 45 years old (SD =16.6; median =42; range: 18–92 years old). Early-onset diagnosis at 35 years of age or younger was found in a third of the population (33.7%), and more than half of the population (67.8%) was diagnosed before the age of 50. Females represented 65.3% of the study population (Table 1) and were diagnosed earlier than were men (mean age 43.1 vs 45.5 years) (P<0.0001).
  | Table 1 Demographic characteristics among patients with CD |
BMI at baseline was recorded for over one-third of the study population only (37.2%). Of those with a record, the mean BMI was 27.9 (SD =6.3), with 65.2% classified as overweight (BMI in the range of 25–30) or obese (BMI >30). Smoking status could be determined in 98.7% of the patients. About half of them (44.3%) declared they had never smoked, and 18.9% of patients were current smokers, defined in their most recent smoking status as “current smoker” at baseline.
Socioeconomic status was assessed and scored to indicate patients’ deprivation level geographically, with 1 being least deprived and 5 being most deprived. This was recorded in 95.6% of the patients, of which 22.9% came from the least-deprived category, followed by 21.6% from category 2, 21.2% from category 3, 19.3% from category 4, and 15.2% from category 5, the most-deprived area. This distribution was consistent with that of the overall THIN population (data provided by Cegedim Strategic Data Medical Research UK (CSD MR UK).
Overall, most patients (82.5%) did not have any of the comorbidities investigated. Depression in the last year before diagnosis was the most common comorbidity, present in 8.0% of the cohort, followed by acquired brain injury, present in 5.2% of patients, and anxiety or sleep problems in the last 12 months, present in 3.6% of patients. In older patients aged above 65 years, prevalence of depression in the last 12 months was lower (3.9% in the age group 66–80 years; 7.2% in the age group >80 years).
Health care resource utilization
Primary care utilization was high in both years (Table 2). In the first year, 99.2% of patients attended the GP practice at least once, and of those who visited the GP at least once, the average number of visits was 6.2 (SD =5.5; median =5). In the second year, 88.5% had at least one visit and attended, on average, 5.9 times (SD =5.3; median =4). In the first year, 43.3% of patients had at least one nurse visit (at the GP practice, telephone, and letter consultations), with 2.5 visits on average (SD =2.6; median =2); there was a similar number of visits in the second year (41.9% of patients had at least one nurse visit; mean =2.7 visits; SD =4.5; median =2). Overall, GPs made a referral to the specialist for 49.0% of patients during the first year. Not all referral records had information available about the specialty to which patients were referred; this was available for 71.7% of all referrals made. The most common specialists to whom patients were referred at least once were orthopedic surgeons (8.7% of the population), followed by Ear, Nose, and Throat (ENT) specialists (4.2%), neurologists (4%), rheumatologists (2.8%), and psychiatrists (2.6%). Referrals for blood samples and laboratory tests (department of pathology) were found in 5.7% of the patients, and referrals to pain management specialists were found in only 0.4% of the patients. During the second year, the proportion of patients referred to specialists was very similar to the first year (50.5%), and 67.7% of all referrals had information available about the referral specialty. By specialist, the proportion of patients who had visited them at least once was very similar to that in the first year.
  | Table 2 Health care resource use after diagnosis |
A total of 1.4% and 1.3% of patients had a record of having been admitted to hospital in the first and second year after diagnosis, respectively, with median attendance to hospital of once per year. The reason for hospitalization was not available in THIN. Read codes indicating neurosurgeries were also explored for deep brain stimulation and selective peripheral denervation, and less than 1% of patients were found to have undergone these procedures.
Regarding physical therapy, in the first year after diagnosis 15.9% of patients were reported to have had at least one referral or visit with the physiotherapist. In the second year, the percentage of patients with CD with a record of physiotherapy was 9.9%. A very small proportion of patients were referred to occupational or speech therapy during the first 2 years after diagnosis.
Pharmacological treatment
The most common medications treating CD were reported separately for the first and second year after diagnosis (Table 3).
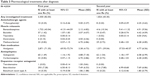  | Table 3 Pharmacological treatments after diagnosis |
In the first year after diagnosis, 82.0% of patients were prescribed with at least one of the investigated treatments. Most patients were prescribed treatment to minimize pain, which is often regarded as the most disabling symptom for patients with CD.24 More than 70% of patients used pain medication (analgesics) and received, on average, 3.4 prescriptions per patient (SD =4.7, range: 1–72). In total, 45.4% of patients were prescribed with muscle relaxants, of which the vast majority (94.8%) received benzodiazepines, at a mean of 2.1 prescriptions per patient (SD =4.8, range: 1–102). Oral baclofen was prescribed to 1.4% of patients in the first year. Beta-blockers were prescribed to 7.3% of patients, antiepileptics to 2.3%, and anticholinergic agents or dopamine receptor antagonist to less than 1% of patients. Within 1 year post–index period, 43.4% of patients received only one type of the studied medications, 33.7% received two types, and the remaining 4.8% were prescribed three or four different medication types.
In the second year after diagnosis, the proportion of patients treated with any of the investigated medications decreased to less than half of patients (45.3%). Within the group of patients with at least one of the study prescriptions recorded, the most commonly used medications remained the same as in the first year – analgesics and benzodiazepines. However, the percentage of patients using these medications dropped to 39.0%, for analgesics, and to 10.3%, for benzodiazepines. The proportion of patients receiving any of the other study medications remained similar to that in the first year.
Discussion
This study used a population-based primary care database to describe sociodemographic and clinical characteristics as well as health care resource utilization in patients with CD in the UK. A total of 4,024 patients with CD were identified between January 1, 2007 and January 31, 2011. Based on the prior incidence estimates of between 8 and 12 cases per million person-years,4,25,26 the number of cases identified in THIN was larger than that previously reported in the literature. However, prior studies were considered to have low estimates27 owing to the way they had been designed. They mostly evaluated patients who attended secondary care facilities specializing in treatment of this condition, whereas in THIN, a wider population was included, namely all subjects coded by their GP as “spasmodic torticollis”, and in the UK, some of them would be managed in the primary care setting only.
The findings suggest that the proportion of female patients diagnosed with CD was higher than for male patients, and females had an earlier average age of onset, which is consistent with findings from the wider literature.4–9,28 Comorbidities were frequently reported in patients with CD, and several publications have focused on anxiety and depression.13,29,30 Depression was the most common condition in patients with CD, present in 8.0% of the cohort within 12 months prior to diagnosis of CD, and increasing up to 32.7% when the whole patient history was used.
In the 2 years after diagnosis, almost all patients were seen by their GP. In the first 12 months after diagnosis, 99.2% of patients were seen by their GP at least once, while in the second 12 months after diagnosis 88.5% were seen by their GP at least once. This is consistent with the UK setting where GPs are the primary point of contact for patients, acting as the gatekeeper of the health care system. Of those patients attending at least once, the average number of visits was similar in the first 12 months (6.2 visits) to that in the second 12 months (5.9 visits). The proportion of patients referred to specialists was similar across the 2 years after diagnosis; however, the proportion of patients referred to a neurologist was found to be low. Referrals in the UK are needed for the first interaction with the specialist, but afterwards, follow-up visits for the same condition do not require additional referral by the GP. One possible explanation is that GPs would refer patients to the neurologist when first symptoms occur and the specialists would feed back the diagnosis to the GP for a shared management of the patient. Therefore, after the diagnosis of CD observed in the primary care, the number of referrals to the neurologist is expected to be low. Health care resource utilization was compared with that of all patients registered in THIN, which is representative of the UK. After adjusting by age, sex, and socioeconomic status, the usage of primary care resources was found to be similar to that of other patients. Secondary care, as captured in the database, was found to be higher in patients with CD compared with that in the rest of the population in THIN.
Oral medications were generally prescribed by the GP, including treatment continuation for chronic conditions that were initiated in the specialist setting. The most common treatments for CD were analgesics and benzodiazepines. Pain has been reported in the literature as affecting up to 75% of patients with CD,24 which appears to be consistent with the high prescription rates of analgesics. However, in THIN, only the data on prescription type are available, whereas the reason for prescription cannot be determined. Therefore, the rates of prescription of analgesics cannot be directly linked to the diagnosis of CD. Surgical treatments were found in very few patients. These usually involved an interdisciplinary team, involving neurologists, neurosurgeons, psychiatrists, and neuropsychologists, who might not consistently report back the data to the primary care physicians, so the low numbers of surgical treatments could be due to this information being underreported.
Overall, results were consistent to those self-reported in the First International Cervical Dystonia Patient Survey of Patients with Cervical Dystonia.31 Patients reported that the symptoms of CD affected them in the following ways: “experienced pain” (66%), “depression and mood alteration” (61%), “lack of sleep” (45%), “not participating in leisure activities” (41%), “having to give up work” (38%), “deterioration in family relationship” (36%), “loss of independent living” (32%), “not able to shop” (25%), and “increased alcohol intake” (15%). Treatments chosen or prescribed (at any time) included: BoNT-A (86%), oral medication (53%), physiotherapy (31%), psychological support (11%), and surgery/deep brain stimulation (9%).
There are limitations associated with this study, which suggest the results should be interpreted with appropriate caution. This study was descriptive in nature, and although the health care resources that were investigated are those associated with CD, given the nature of the database and lack of detailed reason for prescription or visit, it was not possible to specifically attribute them to CD. This is a common limitation in retrospective studies. Additionally, detailed data on resources from the secondary care setting are not well captured in THIN, including medical treatment and procedures. Read codes related to treatment with BoNT-A were investigated as part of this study, and only 0.35% and 0.29% of the patients recorded in the first and second year after diagnosis, respectively, were found to have one of the Read codes. This could reflect the initial stages of the disease in the first 2 years after diagnosis or a predominance of patients with CD with mild symptoms. Still, percentages were lower than expected for this patient population, and it is possible that there were a number of treatments with BoNT-A that were not captured within the database, which could account for the low numbers. Further prospective studies from supplementary data sources that capture more elements of secondary care are needed to fully understand the overall economic burden associated with CD.
Despite the limitations, this study has a number of strengths. First, THIN records are broadly representative of the UK population in terms of age, sex, and geographical locations, and have been widely used for many cohort studies in many conditions. Additionally, the use of real-world data provides a comprehensive picture of how patients are managed in the UK, rather than being restricted to one specific hospital or geographic region. The data provided a large sample size for cross-sectional research, containing extensive data on comorbidities, referrals, and primary care administered treatments. This study is the first to provide estimates of the utilization of health care resources as indication of the economic impact related to management of individuals with CD in the UK. First and second year resource utilization were described separately.
Conclusion
This study contributes to the estimation of health care resource utilization as indication of the economic impact related to management of CD in the UK. A large number of cases of CD were identified retrospectively in the primary care setting, and primary care utilization was found to be comparable with the general population. For the most part, dystonia is a lifelong disorder, with the presence and severity of symptoms fluctuating over time. Future research on the overall burden of the disease should include a longer time horizon, to understand how the burden evolves as the condition progresses. Appropriate management of the condition is the key to controlling health care resource utilization in the context of a public health system, like the National Health Service (NHS) in the UK. To describe the complete burden of CD, indirect costs of employment disability as a result of CD (documented in a number of studies) and quality of life should be included.
Acknowledgments
The authors would like to thank Hannah Kurth (Global Market Access and Pricing, Ipsen Pharma), and Dimitra Lambrelli and Andrew Cox (Research Scientists, Evidera) for their valuable input throughout the study, and Sharon MacLachlan (Research Associate, Evidera) for excellent data programming work. The authors are also grateful to Evan Davies (Research Associate, Evidera) for his revision and edits on the manuscript.
Disclosure
The study was funded by Ipsen Pharma. Ms Raluy-Callado, Dr Wasiak, and Dr Wang are full-time employees of Evidera. Dr Dinet and Dr Gabriel are Ipsen Pharma employees. The authors report no other conflict of interest in this work.
References
Simpson DM, Gracies JM, Graham HK, et al; Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Assessment: Botulinum neurotoxin for the treatment of spasticity (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2008;70(19):1691–1698. | ||
Van Zandijcke M. Cervical dystonia (spasmodic torticollis). Some aspects of the natural history. Acta Neurol Belg. 1995;95(4):210–215. | ||
Epidemiological Study of Dystonia in Europe (ESDE) Collaborative Group. A prevalence study of primary dystonia in eight European countries. J Neurol. 2000;247(10):787–792. | ||
Nutt JG, Muenter MD, Aronson A, Kurland LT, Melton LJ. Epidemiology of focal and generalized dystonia in Rochester, Minnesota. Mov Disord. 1988;3(3):188–194. | ||
Duffey PO, Butler AG, Hawthorne MR, Barnes MP. The epidemiology of the primary dystonias in the north of England. Adv Neurol. 1998;78:121–125. | ||
Erjanti HM, Marttilla RJ, Rinne UK. The prevalence and incidence of cervical dystonia in south-western Finland. Mov Disord. 1996;11(Suppl 1):S215. | ||
Nutt JG, Muenter MD, Melton LJ, Aronson A, Kurland LT. Epidemiology of dystonia in Rochester, Minnesota. Adv Neurol. 1988;50:361–365. | ||
Soland VL, Bhatia KP, Marsden CD. Sex prevalence of focal dystonias. J Neurol Neurosurg Psychiatry. 1996;60(2):204–205. | ||
Chan J, Brin MF, Fahn S. Idiopathic cervical dystonia: clinical characteristics. Mov Disord. 1991;6(2):119–126. | ||
Jankovic J, Leder S, Warner D, Schwartz K. Cervical dystonia: clinical findings and associated movement disorders. Neurology. 1991;41(7):1088–1091. | ||
Jahanshahi M, Marion MH, Marsden CD. Natural history of adult-onset idiopathic torticollis. Arch Neurol. 1990;47(5):548–552. | ||
Jankovic J. Treatment of dystonia. Lancet Neurol. 2006;5(10):864–872. | ||
Swope D, Barbano R. Treatment recommendations and practical applications of botulinum toxin treatment of cervical dystonia. Neurol Clin. 2008;26 Suppl 1:S54–S65. | ||
Comella CL, Thompson PD. Treatment of cervical dystonia with botulinum toxins. Eur J Neurol. 2006;13 Suppl 1:S16–S20. | ||
Brin MF, Benabou R. Cervical Dystonia (Torticollis). Curr Treat Options Neurol. 1999;1(1):33–43. | ||
Greene P, Shale H, Fahn S. Analysis of open-label trials in torsion dystonia using high dosages of anticholinergics and other drugs. Mov Disord. 1988;3(1):46–60. | ||
Tassorelli C, Mancini F, Balloni L, et al. Botulinum toxin and neuromotor rehabilitation: An integrated approach to idiopathic cervical dystonia. Mov Disord. 2006;21(12):2240–2243. | ||
Adler CH, Kumar R. Pharmacological and surgical options for the treatment of cervical dystonia. Neurology. 2000;55(12 Suppl 5):S9–S14. | ||
Vidailhet M, Vercueil L, Houeto JL, et al; French Stimulation du Pallidum Interne dans la Dystonie (SPIDY) Study Group. Bilateral deep-brain stimulation of the globus pallidus in primary generalized dystonia. N Engl J Med. 2005;352(5):459–467. | ||
Brefel-Courbon C, Simonetta-Moreau M, Moré C, et al. A pharmacoeconomic evaluation of botulinum toxin in the treatment of spasmodic torticollis. Clin Neuropharmacol. 2000;23(4):203–207. | ||
Dodel RC, Kirchner A, Koehne-Volland R, et al. Costs of treating dystonias and hemifacial spasm with botulinum toxin A. Pharmacoeconomics. 1997;12(6):695–706. | ||
Burbaud P, Ducerf C, Cugy E, et al. Botulinum toxin treatment in neurological practice: how much does it really cost? A prospective cost-effectiveness study. J Neurol. 2011;258(9):1670–1675. | ||
Blak BT, Thompson M, Dattani H, Bourke A. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care. 2011;19(4):251–255. | ||
Lowenstein DH, Aminoff MJ. The clinical course of spasmodic torticollis. Neurology. 1988;38(4):530–532. | ||
Marras C, Van den Eeden SK, Fross RD, et al. Minimum incidence of primary cervical dystonia in a multiethnic health care population. Neurology. 2007;69(7):676–680. | ||
Claypool DW, Duane DD, Ilstrup DM, Melton LJ. Epidemiology and outcome of cervical dystonia (spasmodic torticollis) in Rochester, Minnesota. Mov Disord. 1995;10(5):608–614. | ||
Defazio G, Jankovic J, Giel JL, Papapetropoulos S. Descriptive epidemiology of cervical dystonia. Tremor Other Hyperkinet Mov (N Y). 2013;3. | ||
Queiroz MR, Chien HF, Barbosa ER. Quality of life in individuals with cervical dystonia before botulinum toxin injection in a Brazilian tertiary care hospital. Arq Neuropsiquiatr. 2011;69(6):900–904. | ||
Ben-Shlomo Y, Camfield L, Warner T; ESDE collaborative group. What are the determinants of quality of life in people with cervical dystonia? J Neurol Neurosurg Psychiatry. 2002;72(5):608–614. | ||
Müller J, Kemmler G, Wissel J, et al; Austrian Botulinum Toxin and Dystonia Study Group. The impact of blepharospasm and cervical dystonia on health-related quality of life and depression. J Neurol. 2002;249(7):842–846. | ||
Comella CL, Bhatia K. An international survey of patients with cervical dystonia. Presented at: Second International Congress on Treatment of Dystonia; May 8–13; 2013; Hanover, Germany. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
