Back to Journals » Drug Design, Development and Therapy » Volume 9
1-1-12 one-step wash-in scheme for desflurane low flow anesthesia: performance without nitrous oxide
Authors Sathitkarnmanee T , Tribuddharat S, Nonlhaopol D, Thananun M, Somdee W
Received 27 November 2014
Accepted for publication 23 December 2014
Published 17 February 2015 Volume 2015:9 Pages 977—981
DOI https://doi.org/10.2147/DDDT.S78233
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Shu-Feng Zhou
Thepakorn Sathitkarnmanee, Sirirat Tribuddharat, Duangthida Nonlhaopol, Maneerat Thananun, Wilawan Somdee
Department of Anesthesiology, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Background: We reported a 1-1-12 wash-in scheme for desflurane-nitrous oxide (N2O) low flow anesthesia that is simple, rapid, and predictable. There remain some situations where N2O should be avoided, which limits the generalizability of this wash-in scheme. The objective of our study was to determine the performance of this scheme in contexts where N2O is not used.
Methods: We recruited 106 patients scheduled for elective surgery under general anesthesia. After induction and intubation, wash-in was started with a fresh gas flow of air:O2 1:1 L/min and a vaporizer concentration of desflurane of 12%. Controlled ventilation was then adjusted to maintain PACO2 at 30–35 mmHg.
Results: The alveolar concentration of desflurane (FAD) rose rapidly from 0% to 6% in 4 minutes in the same pattern as observed in our previous study in which N2O was used. An FAD of 7% was achieved in 6 minutes. An FAD of 1% to 7% occurred at 0.6, 1, 1.5, 2, 3, 4, and 6 minutes. The rise in heart rate during wash-in was statistically significant, although not clinically so. There was a slight but statistically significant decrease in blood pressure, but this had no clinical significance.
Conclusion: Performance of the 1-1-12 wash-in scheme is independent of the use of N2O. Respective FADs of 1%, 2%, 3%, 4%, 5%, 6%, and 7% can be expected at 0.6, 1, 1.5, 2, 3, 4, and 6 minutes.
Keywords: low flow anesthesia, wash-in, desflurane, air
Introduction
Low flow anesthesia (fresh gas flow [FGF] ≤1 L/min) is gaining in popularity because of its advantages (vis-à-vis economy, less pollution, and conservation of heat and humidity)1 in addition to the availability of modern anesthetic machines and anesthetic gas monitors. Desflurane, with its properties of low blood and fat solubility and no limitation of FGF even with older CO2 absorbers, is most suitable for low flow anesthesia.2 Low flow anesthesia needs an initial wash-in phase to build up the required concentration of desflurane in the circle circuit (FID) and alveoli (FAD).3 Most reported wash-in schemes need a very high FGF or vaporizer concentration of desflurane, yet achieve only some of the targeted FAD.2,4,5 There is one scheme that can achieve every FAD, but it is a complex logistic regression equation needing a computer to perform the calculation,6 so is inconvenient for everyday use. Recently, the authors reported a simple, single step 1-1-12 wash-in scheme using an FGF of N2O:O2 1:1 L/min and desflurane 12%, that can rapidly yield every FAD from 1% to 6% within 4 minutes without tachycardia.7 Although N2O is widely used because of its desirable effects (eg, analgesia and additive effect to the minimum alveolar concentration [MAC] of desflurane), there are still some situations where N2O should not be used,8–11 which effectively limits the generalizability of this scheme. The objective of the present study was to evaluate the 1-1-12 wash-in scheme in situations where N2O is currently excluded.
Materials and methods
This study was approved by the institutional review board of Khon Kaen University (HE561247) and was registered at www.clinicaltrials.gov (NCT01348984). All patients gave their written informed consent before enrollment.
This was a descriptive trial. The sample size comprising 106 patients was determined in the same way as in our previous related study.7 We included patients with an American Society of Anesthesiologists physical status of I or II, aged 16–64 years, and scheduled for elective surgery under general anesthesia with endotracheal intubation and controlled ventilation. Patients with pulmonary or cardiac disease, a body mass index >30 kg/m2, or a contraindication to use of succinylcholine were excluded.
All patients were managed by standard intraoperative monitoring and care in the same way as in our previous study.7 They were monitored with electrocardiography, pulse oximetry, noninvasive blood pressure measurement, capnography, and anesthetic gas analyzing equipment. The anesthetic machine, integrated with an anesthetic gas analyzer, used in this study was a Primus (Dräger AG, Lübeck, Germany). We used a standard circle circuit with a soda lime absorber. Each patient’s heart rate and blood pressure were recorded before induction as a baseline measurement. The patients were then premedicated with intravenous fentanyl 1 μg/kg and induced with propofol 2 mg/kg. Intubation was facilitated with succinylcholine 1.5 mg/kg. Ventilation was controlled using an FGF of air:O2 1:1 L/min and desflurane 12%. The initial ventilator setting was at a tidal volume 7 mL/kg and a respiratory rate of 12 per minute adjusted to keep the PACO2 around 30–35 mmHg. The time to achieve an FAD at 1%, 2%, 3%, 4%, 5%, 6%, and 7% was recorded as the primary outcome. FID, heart rate, and blood pressure at each FAD were also recorded. After an FAD of 7% was achieved, FGF was reduced to 0.5–1 L/min and desflurane adjusted according to the judgment of the anesthesiologist.
Statistical analysis
The statistical analysis was performed using Statistical Package for the Social Sciences for Windows version 16.0 software (SPSS Inc, Chicago, IL, USA). Continuous demographic data are presented as the mean ± standard deviation and the categorical data as the number of patients (percentage). The primary outcome is presented as the mean ± standard deviation and 95% confidence interval. The unpaired Student’s t-test was used to compare the time and FID to achieve each FAD in this study, consistent with our previous study.7 Heart rate and blood pressure values at different time points were compared using repeated measures analysis of variance. P<0.05 was considered to be statistically significant.
Results
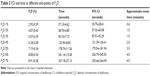
In total, 106 patients participated in and completed the study. The demographic data for these patients are presented in Table 1.
The trajectories of time taken to reach each FAD by each patient during wash-in are presented in Figure 1. The times taken to achieve FAD from 1% to 7% and the 95% confidence intervals are presented in Table 2. Mean times in seconds were converted into approximate time in minutes for practical use. An FAD of 1%, 2%, 3%, 4%, 5%, 6%, and 7% can thus be expected at 0.6, 1, 1.5, 2, 3, 4, and 6 minutes, respectively.
  | Figure 1 Trajectories of time to achieve each FAD during wash-in. |
The rising pattern of FAD and FID is similar to that observed in our previous study,7 except for some statistically but not clinically significant differences at 5%, 6% and 4%, 5%, 6%, respectively (Figures 2 and 3).
  | Figure 2 Rising patterns of FAD during wash-in when N2O was included versus excluded. |
  | Figure 3 Rising pattern of FID during wash-in when N2O was included versus excluded. |
The rise in heart rate during wash-in was statistically but not clinically significant (Figure 4). Blood pressure decreased slightly; this was statistically significant but not clinically so (Figure 5). These patterns are similar to those in our earlier study.7
  | Figure 4 Heart rate at different FAD during wash-in when N2O was excluded. |
Discussion
The pattern of the trajectories of time taken to achieve each FAD in Figure 1 reveals that this scheme has acceptable intrasubject and intersubject variability. Although there are statistically significant differences in the increasing pattern of time and FID at some points of FAD, these are in the order of a few seconds and not clinically significant. The times taken to achieve FAD from 1% to 6% in this study (without N2O as the carrying gas) is the same as that reported in our previous study, which used N2O as a part of FGF.7 The results of the present study show that the performance of the 1-1-12 wash-in scheme is not affected by the use of N2O. The second gas effect of N2O12 does not influence the uptake of desflurane because both N2O and desflurane have nearly the same very low blood-gas solubility (0.47 versus 0.42). We extended the end point of FAD in this study to 7%, which took 6 minutes to achieve, because without N2O, which has an additive effect on the MAC of desflurane,13 a higher FAD may be required to control the depth of anesthesia. The time required to increase FAD from 6% to 7% was 2 minutes, which is double the time required to increase each 1% from 4% to 6%. This may be due to the narrower gradient between FID and FAD at the high end of FAD.
Our scheme requires less FGF, but can achieve each FAD from 1% to 7% within 6 minutes, which is more rapid and simpler than most reported wash-in schemes. Baum et al used an FGF of 4.4 L/min and found that FAD reached 90%–95% of the fresh gas concentration within 10–15 minutes.2 Mapleson reported a spreadsheet model comprising two components: a circle circuit and a 70 kg anesthetized “standard man”, using an FGF equal to the total ventilation with 3 MAC of desflurane that could achieve an FAD of one MAC in 1 minute.4 Hendrickx et al used an FGF of O2:N2O 2:4 L/min with desflurane 6.5% and found that an FAD of 4.5% could be achieved in 15 minutes.5
The aforementioned schemes used higher FGFs yet achieved only some specific FADs. Hendrickx et al thus proposed an empirical model that could be used to predict FGF-desflurane combinations that achieved a target FAD within the first 5 minutes.6 Their model, however, is a complex logistic regression equation requiring a computer to calculate, making it impractical for daily use. In comparison, our scheme is simpler and more practical, and yields a rapid wash-in with an expected FAD from 1% to 7% at 0.6, 1, 1.5, 2, 3, 4, and 6 minutes, respectively. This range of FAD covers the concentration for both balanced and pure inhalation anesthesia. This scheme can be applied with or without N2O.
While Nyktari et al14 reported that a rapid increase in FID to 1.5 MAC without the support of premedication caused a significant increase in airway resistance, we did not find such a problem. The explanation is that, with a lower FGF, an FID of 1.5 MAC was gradually achieved in 7 minutes and fentanyl was used as a premedication.
In the current study, there was a statistically significant but not clinically increase in heart rate and decrease in blood pressure. This result is similar to our previous study using N2O as a carrying gas7 and also consistent with the report by Warltier and Pagel,15 but different from the study by Ebert and Muzi,16 who reported hypertension and tachycardia in healthy volunteers receiving titration of desflurane from 1 to 1.5 MAC following thiopental induction. The explanation is that fentanyl, used as a premedication, attenuates sympathetic stimulation.17 Moreover, the rapid increase in FID in our scheme (to the level exceeding the MAC of desflurane before the therapeutic level of the induction agent is on the wane) maintains the patient in the surgical stage throughout the study without sympathetic overactivity.
The 1-1-12 wash-in scheme has many advantages: simplicity (just one step for setting); coverage (every targeted FAD from 1% to 6% [7% where N2O is omitted]); rapidity (achieving the targets within 0.6 to 4 minutes [6 minutes for 7%]); flexibility (applicable to situations both with or without N2O); safety (wash-in without sympathetic overactivity); and economy (just 2 L/min of FGF and 12% desflurane). After achieving the required FAD, the FGF can be reduced to a low flow anesthesia range of 0.5–1 L/min and the target FAD can be simply maintained by setting the desflurane above the FAD by 1%–2%.3,18
Given that we excluded patients with a body mass index >30 kg/m2, this scheme may not be generalized to such conditions, so further study is required.
Conclusion
The 1-1-12 wash-in scheme using a simple, single step FGF of N2O or air:O2 1:1 L/min and desflurane 12% for low flow anesthesia in patients requiring general anesthesia with endotracheal intubation and controlled ventilation has the same performance with or without N2O. Each concentration of FAD from 1% to 7% can be expected at 0.6, 1, 1.5, 2, 3, 4, and 6 minutes, respectively. The 1-1-12 wash-in scheme covers the FAD required for both balanced and pure inhalation anesthesia. There were nonclinically significant increases in heart rate and decreases in blood pressure during this wash-in period.
Acknowledgments
This study was funded by the Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand. We thank Bryan Roderick Hamman and Janice Loewen-Hamman for assistance with English language presentation of the manuscript via Publication Clinic KKU, Thailand.
Disclosure
The authors report no conflicts of interest in this work.
References
Odin I, Feiss P. Low flow and economics of inhalational anaesthesia. Best Pract Res Clin Anaesthesiol. 2005;19(3):399–413. | ||
Baum J, Berghoff M, Stanke HG, Petermeyer M, Kalff G. Low-flow anesthesia with desflurane. Anaesthesist. 1997;46(4):287–293. | ||
Baum JA. Low-flow anesthesia: theory, practice, technical preconditions, advantages, and foreign gas accumulation. J Anesth. 1999;13(3):166–174. | ||
Mapleson WW. The theoretical ideal fresh-gas flow sequence at the start of low-flow anaesthesia. Anaesthesia. 1998;53(3):264–272. | ||
Hendrickx JF, Dewulf BB, De Mey N, et al. Development and performance of a two-step desflurane-O(2)/N(2)O fresh gas flow sequence. J Clin Anesth. 2008;20(7):501–507. | ||
Hendrickx JF, Lemmens H, De Cooman S, et al. Mathematical method to build an empirical model for inhaled anesthetic agent wash-in. BMC Anesthesiol. 2011;11:13. | ||
Sathitkarnmanee T, Tribuddharat S, Suttinarakorn C, et al. 1-1-12 one-step wash-in scheme for desflurane-nitrous oxide low-flow anesthesia: rapid and predictable induction. Biomed Res Int. 2014;2014:867504. | ||
Becker DE, Rosenberg M. Nitrous oxide and the inhalation anesthetics. Anesth Prog. 2008;55(4):124–130. | ||
Imberger G, Orr A, Thorlund K, Wetterslev, Myles JP, Moller AM. Does anaesthesia with nitrous oxide affect mortality or cardiovascular morbidity? A systematic review with meta-analysis and trial sequential analysis. Br J Anaesth. 2014;112(3):410–426. | ||
Leslie K, Myles PS, M. Chan T, et al. Nitrous oxide and long-term morbidity and mortality in the ENIGMA trial. Anesth Analg. 2011;112(2):387–393. | ||
Myles PS, Leslie K, M. Chan T, et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. Anesthesiology. 2007;107(2):221–231. | ||
Epstein RM, Rackow H, Salanitre E, Wolf GL. Influence of the concentration effect on the uptake of anesthetic mixtures: the second gas effect. Anesthesiology. 1964;25(3):364–371. | ||
Albertin A, Casati A, Bergonzi PC, Moizo E, Lombardo F, Torri G. The effect of adding nitrous oxide on MAC of sevoflurane combined with two target-controlled concentrations of remifentanil in women. Eur J Anaesthesiol. 2005;22(6):431–437. | ||
Nyktari VA, Papaioannou A, Volakakis N, Lappa A, Margaritsanaki P, Askitopoulou H. Respiratory resistance during anaesthesia with isoflurane, sevoflurane, and desflurane: a randomized clinical trial. Br J Anaesth. 2011;107(3):454–461. | ||
Warltier DC, Pagel PS. Cardiovascular and respiratory actions of desflurane: is desflurane different from isoflurane? Anesth Analg. 1992;75 (4 Suppl):S17–S29. | ||
Ebert TJ, Muzi M. Sympathetic hyperactivity during desflurane anesthesia in healthy volunteers. A comparison with isoflurane. Anesthesiology. 1993;79(3):444–453. | ||
Katoh T, Kobayashi S, Suzuki A, Iwamota T, Bito H, Ikeda K. The effect of fentanyl on sevoflurane requirements for somatic and sympathetic responses to surgical incision. Anesthesiology. 1999;90(2):398–405. | ||
Johansson A, Lundberg D, Luttropp HH. Low-flow anaesthesia with desflurane: kinetics during clinical procedures. Eur J Anaesthesiol. 2001;18(8):499–504. |
 © 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2015 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.